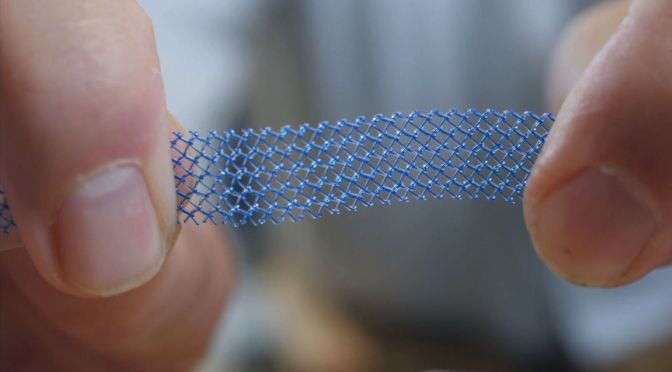
Feature Image of vaginal mesh sourced from:
https://news.sky.com/story/journalist-kath-sansom-was-wreck-after-vaginal-mesh-implant-11086123
Dear Pain Matters blog readers,
This blog post aims to offer hope, inspiration and courage to those women who suffer from severe and ongoing pelvic pain due to failed vaginal mesh implant surgery.
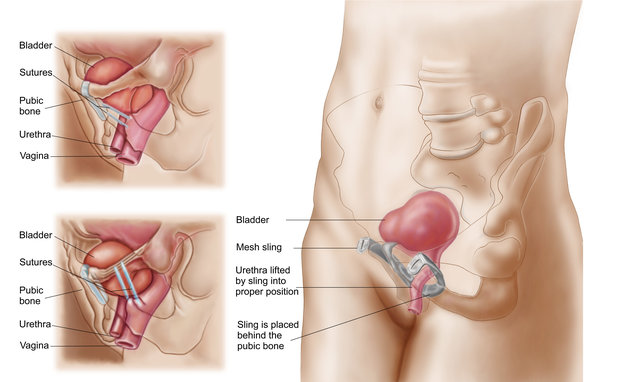
Pelvic mesh implant surgery was often recommended when conservative treatments for prolapse, incontinence and other pelvic conditions failed.
Source: Stocktrek images via Getty Images
Many women were ill-advised of the high risks associated with mesh implant surgery including severe and disabling pelvic pain.
In November 2017, the Therapeutic Goods Administration (TGA) in Australia finally banned 45 pelvic mesh devices including vaginally-implantable prolapse mesh devices and certain mesh slings following the international pelvic mesh fiasco (McCarthy, 2017).
For more information, please watch the 17-minute video by BBC News called ‘NHS sued over vaginal mesh implants’ (18 April 2017).
Several vaginal mesh victims including Kath Sansom (journalist, campaigner and founder of Sling the Mesh) and a urogynaecologist who specialises in mesh excisions are featured in this video.
THREE (3) STUDIES OFFER GOOD NEWS FOR SOME FAILED MESH IMPLANT PATIENTS
Overview
Patients suffering from severe pain and other serious complications due to failed mesh implants may explore whether mesh removal surgery (i.e. mesh excision) is a viable option to remove all or part of the mesh implant.
Click to access ExcisionOfMesh.pdf
https://urogyn.coloradowomenshealth.com/patients/library/transvaginal-mesh-removal
Three (3) mesh removal and/or suburethral tape removal studies, being American, French and Dutch studies, are discussed below:
An American Vaginal Mesh/Suburethral Tape Removal Study
An American study analyzed the results of 123 patients who had surgery to remove vaginal mesh (N=69; the mesh group) or synthetic suburethral tape (N=54; the tape group) in a bid to reduce pain during 2005 to 2013.
The average visual analog score (VAS) score was reduced from 7.9 (before surgery) to 0.9 after removal surgery in the mesh group, as revealed during follow-up 6 to 47 months later.
Meanwhile, the average VAS score decreased from 5.3 (pre-surgery) to 1.5 after removal surgery in the tape group, as revealed during follow-up 6 to 59 months later.
Best of all, 81% of the tape group and 67% of the mesh group were completely pain-free after their respective surgeries!
The authors concluded that if pain is the only reason for surgery to remove either suburethral tape or vaginal mesh, it is likely then that significant pain relief will result following removal surgery (Hou et al, 2014).
A French Mesh Removal Study
A French mesh removal study revealed that mesh can be removed both safely and efficiently in many patients, with operating times averaging only 21 minutes. (NB Some mesh removal operations may require several hours to perform.)
Specifically, 61 of 83 mesh patients underwent complete mesh removal. Fifty-eight (58) mesh excisions were done more than 2 years after the mesh was implanted in the first place (Marcus-Braun and von Theobald, 2010).
A Dutch Mesh Excision Study
A Dutch study analysed 73 mesh-implanted patients who underwent partial or complete mesh excision. Thirty (30) patients had complete mesh removal while 43 patients underwent 51 partial mesh operations.
Prior to their mesh removal surgery, 77% suffered severe pain including vaginal pain, vaginal bleeding/discharge, pain during sex as well as lower abdominal, back, buttock and/or leg pain.
Positive outcomes including symptom relief were achieved for 92% of the 73 patients.
Specifically, 70% of those patients who underwent complete mesh excision and 60% of those who had partial mesh excision enjoyed COMPLETE RELIEF from mesh-related symptoms.
As with all surgeries, there are inherent risks and complications that may be involved with mesh excisions. Furthermore, pelvic organ prolapse or stress urinary incontinence may recur (Tijdink et al, 2011).
Further to Aforementioned 3 Studies
Please note that whilst the results from the American, French and Dutch studies appear very encouraging, it is not known whether these results can be extrapolated and/or whether these results are representative of the norm. More studies are required.*
Each mesh victim who seeks medical advice regarding mesh excision surgery needs to be individually assessed by a highly skilled medical specialist and/or by a mesh removal medical centre (that may or may not be nearby).
Whilst there is always hope, mesh removal surgery may not always be an option due to excessive risks and complications inherent in certain individuals.
However, until one knows for sure, ‘it is usually better to look at the glass as being half full than half empty’.
At the end of the day, botched mesh implants is a collective human issue, and not just an individual problem. As such, we are all in this ‘mesh mess’ together … not just the mesh victims themselves.
Kath Sansom’s Story Including Removal of Vaginal Mesh Implant
Kath Sansom is a journalist and mom of two who used to enjoy high-board diving, boxing and mountain biking.
In March 2015, Kath had a vaginal mesh implant for mild stress urinary incontinence caused by childbirth.
 Kath Sansom, journalist, campaigner and founder of Sling the Mesh
Kath Sansom, journalist, campaigner and founder of Sling the Mesh
Source: https://news.sky.com/story/journalist-kath-sansom-was-wreck-after-vaginal-mesh-implant-11086123
As soon as her mesh sling was implanted, Kath felt pain. In her words,
‘The pain was instant. I struggled to walk. The pain down the backs of my legs felt like really deep, heavy toothache. It hurt me to walk, sit, lie. I couldn’t get any relief. I had cheese-wiring pains in my vagina, burning pain so bad I couldn’t even use a tampon. In the weeks before, I did a boxing class, high-board diving and mountain biking. I went from that to excruciating pain … it gradually got worse and worse.’
Kath felt betrayed because the true risks of vaginal mesh implants were never revealed to her prior to surgery. She said she would have ‘run out the door’ if only someone had said (quoting),
‘You can have this little operation but you might lose your sex life.’
or
‘You can have this little operation and you might not be able to walk – but at least you won’t wee your pants.’
Kath Sansom had her botched mesh sling removed 7 months later. In her words (quoting),
‘I got a lot better, although I’m right up there at the good end of recovery compared with other women. I can still swim. But even so, it’s a new normal. I have to be very careful when putting impact on my legs, I have to be careful how I move. If I overdo things I can end up in pain the next day and having to take strong painkillers. I’ve got all these pain relievers in my bag just in case …’
‘You go from being a healthy mum with a bit of an embarrassing problem, to suddenly your life is turned on its head. And you’ve got to accept that this is now your life because even if you have a mesh removal, you will never go back to the woman you were.’
After her dreadful experience with the now-removed vaginal mesh implant, Kath founded and runs the Sling the Mesh campaign group that has over 7,300 members (Sansom, 2017; Brown, 2018; Sansom, 2018; Briggs, 2019; Sling the Mesh).
Catie’s Story Including Removal of Mesh Implant
The following is a story about Catie in New Zealand who underwent 3 operations in an effort to remove all mesh.
Catie’s pelvic mesh was initially implanted without incident. However, 2 years later, (quoting Catie) ‘[the mesh] was rotting and eroding inside …’, causing pain and discharge. At first, Catie was treated for a potential STD (which wasn’t the case at all) via ‘many courses of metronidazole’, an antibiotic with terrible side effects.
Several years later in March 2011, Catie finally underwent her first mesh removal surgery. The partial mesh excision took 5 hours because (in Catie’s words) ‘[the mesh] was so ‘stuck’ on in bits and the surgeon had a lot of difficulty getting it out’.
By August 2012, Catie had 2 more excision surgeries.
After her third (and hopefully final) excision surgery that involved ‘a good clean out’ and a D&C, (quoting Catie) ‘there [was] no revolting discharge and … no pain’.
In Catie’s view, it may be another year or more before she will have fully recovered. She credits her mesh removal surgeon for being wonderful.
Formerly a triathlete, Catie is struggling to become active again. Nonetheless she is grateful for feeling better after a very long and painful journey.
Catie’s Story:
http://meshdownunder.co.nz/kiwi-stories
Claire Daisley’s Story – Mesh Removal Surgery by Dr Veronikis
Claire Daisley, a 49-year old mother of 3 in Greenock, Scotland, suffered severe pelvic pain following mesh implant for bladder weakness after childbirth 9 years ago in 2010. She used crutches and wheelchairs due to unbearable pain. Climbing stairs was a nightmare. Claire even considered suicide to end all her suffering.
After her mesh implant, Claire became doubly incontinent. Furthermore, she developed osteoarthritis, autoimmune issues and other medical problems.
Following surgery in Scotland to remove only 1/3 of her mesh, Claire was told that it was all gone. Unsurprisingly, her pain and other medical issues persisted.
Claire was then told that both her bowel and bladder had to be removed at the end of July 2019.
Fortunately, Claire received a phone call from Dr Veronikis’ office to fly to the US for complete mesh removal surgery at around the same time. Dr Dionysios Veronikis (aka Dr V) is a Harvard-trained obstetrician-gynecologist who specialises in Female Pelvic Medicine, Reconstructive Surgery, Obstetrics and Gynecology. He is based at the Vaginal Surgery and Urogynecology Institute at Mercy Hospital in St. Louis.
Needless to say, Claire cancelled her bowel and bladder removal surgery in Scotland and instead, flew to the US for complete mesh removal surgery by Dr V.
Dr Veroniki was able to remove all of the remaining mesh (i.e. 13 cm of residual mesh) after a 4-hour operation. Furthermore, her bowel and bladder were saved by Dr V.
Given Claire’s dire circumstances, Dr Veroniki performed the mesh removal surgery for free while generous donors paid for her flights, accommodation and hospital fees.
After waking up from surgery, Claire said,
‘Hi, my surgery is all over. My mesh is gone. 13 cm was removed.
So, back in Scotland [when 1st mesh removal surgery was done], to be told that I had a full mesh removal, that there was none left, is shocking!
Claire continued,
‘I have been, and I’m not home a week yet … there’s a difference in my skin that was almost immediate. So things are starting to happen, from having [all the mesh] removed.
For the first time in 9 years, I actually have hope for the future. And I think it’s something that everybody that’s been mesh-injured deserves.
When you’re in so much pain, you don’t have that hope. It’s just an existence.
Now that this is gone, completely mesh-free, there’s hope for the future.’
Claire added,
‘They have not just changed my life, they have saved my life, and I cannot thank them enough. It is hard to believe that only a few months ago, I was in agony and utter despair. I am transformed.
I’m overjoyed that I did [put my trust in Dr V], and thanks to his skills and the … people who donated money … for me to go to the US, I feel like a new woman.
Dr V must be allowed to help other women like me. I’m the living proof.’
For full story including 4-minute video, see:
- Scott, Marion. Video by Megan McEachern.
Crippled in Scotland, saved in the States … Mesh victim Claire Daisley shares her story in today’s Sunday Post. Sunday Post (8 Sept 2019).
- Scott, Marion. ‘This surgery did not just change my life, it saved my life’. Sunday Post (8 Sept 2019).
- Scott, Marion. World-leading mesh surgeon reveals months of talks have failed to fix his trip to Scotland despite minister’s pledge. Sunday Post (8 Sept 2019).
Disclaimer: The story above is not an endorsement of, nor a recommendation for, Dr Dionysios Veronikis (nor any other doctor or medical specialist, for that matter). This story, nor any other patient story, does not imply medical advice. It is a story, and hence, it should be read as such.
Patients should always see their doctors for their personal medical care.
Estelle’s Story – Another Mesh Removal Surgery by Dr Veronikis
Despite 4 surgeries that only removed part of her polypropylene mesh, Estelle Tasz (38) suffered ongoing pain.
Estelle visited Harvard-trained Dr Dionysios Veronikis for the first time at the Vaginal Surgery and Urogynecology Institute at Mercy Hospital in St. Louis. A few days later on 5 August 2014, Dr Veronikis operated on Estelle to successfully remove all of her remaining polypropylene mesh (i.e. transvaginal mesh). Specifically, Dr V removed 17 cm of residual mesh during the 4.5-hour surgery.
In Estelle’s words,
‘Finally, I was told the truth. Finally, I met a doctor who cares, who is a doctor by all meanings of that definition.’
Estelle continues,
‘I feel empty but I feel full. It’s the weirdest feeling, it’s gone, it’s gone. I have a full life ahead of me and Dr. V gave me hope. He saved my life, as a mom, I can’t thank him enough for that.’
For the full story, see:
Akre, Jane. Estelle Finds Complete TVT Removal. Mesh News Desk (12 August 2014).
https://www.meshmedicaldevicenewsdesk.com/estelle-finds-complete-tvt-removal/
Disclaimer: The story above is not an endorsement of, nor a recommendation for, Dr Dionysios Veronikis (nor any other doctor or medical specialist, for that matter). This story, nor any other patient story, does not imply medical advice. It is a story, and hence, it should be read as such.
Patients should always see their doctors for their personal medical care.
WARNING – DO NOT UNDERGO RISKY MESH IMPLANT SURGERY
Many Patients Including an Australian Woman, Jan Wise, Suffer from Pain and Other Complications Following a Botched Mesh Implant
ALL WOMEN, both young and young-at-heart, should be DISCOURAGED from undergoing surgical mesh implants in the first place. Full stop. End of story.
The high risks and serious complications can be catastrophic, post-mesh implant surgery. Mesh implants can cause permanent, disabling and incapacitating pelvic injuries as well as severe, intractable pelvic pain.
Quoting Jan Wise (who now suffers from back and leg pain thanks to a botched implant surgery involving a pig intestine pelvic mesh device in 2012):
‘[I am] rotting from the inside … shooting electrical shock pain from my lower body up through to my head … hoping the thoughts of the nightmare won’t take up too much of [every] day. I allow myself only one period of sadness and crying per day’ (McCarthy, 2017).
Post-implant, in addition to severe pain, Jan suffers ongoing incontinence, a collapsed vagina, (quoting Jan) ‘putrid seroma discharge’ and ‘pelvic discharge with a foul smell’ as well as loss of intimacy with her husband. In her words, ‘It’s a dreadful mess down there.’
Some women require pain killers and benzodiazepines as well as regular catheterisation (due to a lost ability to urinate following a failed implant). Many suffer chronic incontinence together with ongoing urinary tract and vaginal infections, discharge and granulomas. Others require enemas for chronic bowel problems. Punctures or lacerations of vessels, nerves, bladder, urethra, bowel, organs and other structures may occur. Mesh implants often erode into the vagina rendering sex impossible with their husbands or partners.
In some instances, exposed mesh may even cause pain and injury to the male partner during intercourse (McCarthy, 2017; Stern, 2017 – in German).
Sadly, the list of mesh-related severe complications never seems to end.
A Young Canadian Mom, Chrissy Brajcic, Loses Her Life Due to Mesh Complications
One Canadian mother of two young children has died at only 42 due to complications including heart failure and sepsis following pelvic mesh surgery to treat childbirth-induced incontinence (McCarthy, 2017).

Chrissy Brajcic (deceased at only 42 following mesh implant complications)
Source: https://www.independent.co.uk/news/uk/transvaginal-vaginal-mesh-surgery-stress-urinary-incontinence-sui-uti-tvt-antiobiotic-resistance-a8092006.html
A Canadian Woman, Nonie Wideman, Changes her Mind About Committing Suicide Following Emergency Mesh Removal Surgery
Believing to be too great a burden to their family and friends and after giving up hope altogether, some mesh victims commit suicide to end it all (McCarthy, 2017).
A woman from BC, Canada, Nonie Wideman, had emergency surgery that successfully removed the intact mesh only. Sadly, the countless, small eroded mesh fibre pieces could not be surgically removed.
Despite intact mesh removal surgery, Nonie still suffers from chronic pelvic and low back pain including burning pain and inflammation. This is likely due to the numerous tiny pieces of eroded mesh fibres that still remain within her pelvic area.
The good news is that Nonie is no longer contemplating suicide. Instead, she is now an advocate for women suffering from mesh-related pain, disability and disfigurement.
In Nonie’s words,
‘Women are often not believed about how mesh is causing them pain or how much pain the mesh is causing them … We do … suicide watches when women start talking like they’re done, they’re finished, they can’t go on anymore’ (Akre, 2012; Favaro, 2018; Favaro & St. Philip, 2019; Welk et al, 2019).
Many Men Also Suffer Pain and Other Complications Following Botched Hernia Mesh Surgery
Over a dozen hernia patients, mainly men, in Australia suffer severe pain, agony, depression and other complications following botched hernia mesh implant surgery.
The following men share their failed hernia mesh implant stories:
John Coady
John Coady underwent hernia-repair surgery in the mid-1990’s. While at work in early 2010, John suffered a mesh-related complication for the first time. Sadly, the follow-up mesh surgery was a complete disaster and immediately resulted in constant pain and other problems. Quoting John,
‘Before the surgery I was happy, worked six days a well and was always busy … Now I am on morphine and just sit around in pain … After the surgery, my entire groin area including my penis and scrotum was black and I was in excruciating pain … It was like I’d been punched in the genitals. They were just black and just swollen beyond recognition … As the weeks turned into months, I was still suffering from immense pain and suffering.’
The surgeon was unable to alleviate the mesh-related pain and other medical issues despite John seeing the surgeon at least once a week for more than 6 months.
In John’s words,
‘… after about six months, the surgeon told me that there was nothing wrong with me … [adding] ‘I’ve done my job’ and to go away.‘
Dominic’s ‘Five Years of Hell’ Following Failed Hernia Mesh Surgery
Following a botched hernia-mesh operation in 2013, Dominic (46) was left with (quoting) ‘nothing but problems with my bladder’ including pain, incontinence and urine odour. Consequently, his social life including intimacy was virtually non-existent.
George
George, another hernia mesh victim, stated that 2 years after mesh surgery, ‘the mesh got tangled with [his] bowel. He added:
‘I was vomiting this black stuff and I had a tube down my throat. I was in hospital for a week … surgeon … remove[d] all the mesh that was in my stomach. Since then, hernias kept popping out …’
Phil
Phil suffered ongoing pain in his right leg since undergoing mesh implant surgery to repair hernia years ago.
Successful Mesh-Free Surgery for Bob Wolf, Hernia Patient
While most failed mesh implants affect women, some men also suffer following hernia mesh implants.
A mesh-free hernia surgery that was developed by an American surgeon, Dr Mohan Desarda, is now performed by many clinicians.
One satisfied American patient, Bob Wolf, underwent mesh-free hernia surgery 3 years ago in Las Vegas. He decided to have no-mesh hernia repair after his friends told him about their pain and suffering following hernia mesh implant.
In his words,
‘I am 76, running full speed, every day at work and play’
(Wakatama, 2018).
WHAT OPTIONS EXIST, POST-MESH IMPLANT?
If chronic pelvic pain persists, surgical removal of the implanted mesh may be the only effective treatment option for some patients (see aforementioned American, French and Dutch studies). Unfortunately, it may not always be possible to remove all of the mesh without also damaging nearby organs and tissues. In other words, there may be residual mesh that is simply too risky to remove.
OPTIONS TO CONSIDER OTHER THAN MESH IMPLANT SURGERY
Options to try before even thinking about the unthinkable vaginal mesh implant surgery include:
Non Invasive Options
- Pelvic floor exercises, also known as Kegel exercises (named after Arnold Kegel, a US gynaecologist). Kegel exercise can be taught and supervised by a physiotherapist or continence adviser, and done daily at home (Ward, 2018);
- Yoga and pilates that aim to strengthen the pelvic regions;
- Acupuncture for stress urinary incontinence (e.g. Hui Yin acupoint, CV1, Meeting of Yin) ** *** (Kim et al, 2011; Zhu, 2011);
- Incontinence pads (many women opt for this non-invasive option);
- Substitute action sports (e.g. soccer, tennis) for gentler physical activities that may lead to less ‘leakage’ … and don’t stress if there is residual ‘leakage’. After all, that is what incontinence pads and showers are for;
- Maintain a healthy diet, lose weight, stop smoking and ensure good quality of sleep. This is important for optimum autonomic nervous system function including high vagal output throughout the body including in the pelvic region; and
- If concerned, see your family doctor.
Surgery Without Mesh Implant
- Surgery that does not involve mesh implants, in particular, synthetic mesh implants (Bang & Belal, 2016).
In conclusion, please avoid vaginal mesh implants altogether. The risk is too high that severe pelvic pain and other serious injuries may result, post-mesh implant (Heymann et al, 2019).
IS SURGERY TO REMOVE BOTCHED MESH IMPLANTS A VIABLE OPTION FOR SOME PATIENTS?
Like all surgeries, removal of failed mesh implants has inherent risks. As such, some mesh victims may prefer not to consider excision surgery.
Mesh removal surgery may not be in the best interest of mesh victims where the risk of injury is high.
Having said that, mesh victims are encouraged to seek medical advice from urogynaecologists and other medical professionals who specialise in mesh excisions.
A Urogynaecologist in the UK Talks About Vaginal Mesh
A urogynaecologist in the UK named Dr Sohier (Suzy) Elneil, has performed over 250 tension-free vaginal tape (TVT) removal surgeries since 2004. This plastic implant is often used for incontinence.
When Dr Elneil met her first mesh patient with severe pelvic pain in 2004, the mesh implant (TVT) had already disintegrated. Following complex surgery to remove the degraded mesh, the patient was finally pain free and able to return to a normal life.
Dr Elneil described another patient, a lawyer who suffered severe pain since undergoing a mesh implant 6 weeks earlier. By the time Dr Elneil saw her, the lawyer was no longer able to work. Alarmingly, she was also suicidal.
Quoting Dr Elneil,
‘As I was operating on her, I could see the tape was embedded into the tissues and there was ulceration in places — doing the surgery was not nice. I kept thinking: ‘How did it get this bad in six weeks?’. Cases like this keep me going — why in this day and age women should be suffering so makes me very angry.’
Dr Elneil describes mesh removal surgery as,
‘…really hard surgery because the mesh gets embedded in the muscles and everywhere. Even though we scan our patients, you never know what you will find until you open the lady up — and sometimes it can be quite upsetting. To be honest, on occasions I feel bereft because I feel so emotional about it; you realise how much this woman must have been suffering.’
In reply to the journalist’s question about when she’d last had a proper holiday, Dr Elneil replied,
‘But if I go on a long break, it means more women might be left waiting in pain, and I can’t have that’ (Brown, 2018; Elkins, 2018).
There are a number of compassionate urogynaecologists, mesh removal surgeons and other medical professionals who specialise in mesh excision. Please see your doctor if you need a referral.
Disclaimer: The story above is not an endorsement of, or a recommendation for, Dr Sohier (Suzy) Elneil (nor any other doctor or medical specialist, for that matter). It is merely a story, and hence, it should be read as such only. (References are provided.) Patients should see their doctors for referrals to specialists, if they wish to do so.
SUMMARY
Australian Senator, Derryn Hinch, once stated ‘Transvaginal mesh is one of Australia’s greatest medical scandals’ (Marwick, 2017).
Others call it ‘the new thalidomide’.
Still others say, ‘Transvaginal mesh is the biggest scandal affecting women since thalidomide’.
Dr Dionysios Veronikis, obstetrician-gynaecologist (mentioned earlier), stated,
‘…mesh is the single darkest chapter in gynaecological surgery and I will do all I can to help free as many women as possible from pain (Scott, 2019).
Dr Veronikis continues,
‘Mesh prolapse kits were just a bad idea. I don’t kow why so many went down that road. With all those mesh arms and a massive amount of mesh and the one size fits all approach. Every woman is different … [mesh prolapse kits] are defectively designed’ (Akre, 2014).
When asked why he never implanted a vaginal mesh device, Dr Frank Gamberdella (1943 – 2019), gynaecologist, Santa Barbara (50 years of clinical experience), replied,
‘I felt it in my hands, and it wasn’t a device that belonged near the vagina.’ Wise man!
Dr Gamberdella belonged to a generation of physicians who were trained to offer autologous slings (i.e. sourced from self) for the treatment of stress urinary incontinence and non-mesh surgery for pelvic organ prolapse. Mesh should be banned altogether and consideration should be made to return to Dr Gamberdella’s non-mesh surgeries (Survivors with Catastrophic Pain, 2019; Isbert et al, 2003; Bang & Belal, 2016; Baylón et al, 2017; Heymann et al, 2019).
Legal class action suits exist all around the world including lawsuits involving more than 100,000 women in the US alone. Legal bills are expected to exceed $20 billion. This clearly demonstrates the unacceptably high risks of mesh implants.
Vaginal mesh is no longer used in Australia, Ireland and Scotland (Berger, 2019).
To protect all women, mesh implant operations should be banned altogether (McCarthy, 2017). The risks of mesh surgery including disabling pelvic pain, compromised or non-existent sex life, loss of enjoyment of life, suicide and death certainly outweigh any purported benefits.
Finally, women who are adversely affected by pelvic pain due to mesh implants may consider whether mesh excision is an option. In other words, if chronic pelvic pain persists, surgical removal of the implanted mesh may be the only effective treatment option for some patients (see aforementioned American, French and Dutch studies).
It may not be possible to remove all of the mesh without also damaging nearby organs and tissues in some women. There may be residual mesh that is simply too risky to remove. Thus, mesh removal may not be an option for some patients.
I hope that this blog post (that also mentions 3 mesh removal studies, being American, French and Dutch, may offer light at the end of a very long dark tunnel for some women.
Remember that you are NOT alone! As a global community, we are ALL in this together! If you are a mesh implant victim, please reach out for support.
Please help spread the word that this mesh mess is no longer acceptable. Specifically, synthetic mesh implants should be banned altogether.
Sabina Walker
Blogger, Pain Matters (in WordPress)
PS If you believe that this information may help someone, please share this blog post via Twitter, LinkedIn, Facebook, etc.
And please tell this person to never, ever give up!
KEY
* If I find additional mesh removal studies, I will add another blog post to highlight these studies. If you are interested in my updates, just ‘Follow’ this blog and/or my Twitter.
** Acupuncture Helps Bladder Control, Stops Leakage. HealthCMi (12 October 2016).
*** Reiki Master Attunement Exercise
https://www.liannegraham.com/wp-content/uploads/2017/03/Hui-Yin-Exercise.pdf
REFERENCES
Hope for Mesh Patients
Medical Papers and Articles – Corrective Surgery to (Partly or Fully) Reverse Failed Vaginal Mesh Implants
An American Mesh Removal Study
(1) Hou et al. Outcome of transvaginal mesh and tape removed for pain only. J Urol (Sept 2014); 192(3): 856-60.
doi: 10.1016/j.juro.2014.04.006.
https://www.ncbi.nlm.nih.gov/pubmed/24735934
A French Mesh Removal Study
(2) Marcus-Braun, N and von Theobald, P. Mesh removal following transvaginal mesh placement: a case series of 104 operations. Int Urogynecol J. (April 2010); 21(4): 423-30.
doi:10.1007/s00192-009-1050-3.
https://www.ncbi.nlm.nih.gov/pubmed/19936589
A Dutch Mesh Excision Study
(3) Tijdink et al. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Int Urogynecol J. (Nov 2011); 22(11): 1395-404.
doi:10.1007/s00192-011-1476-2.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3187855/
Other Papers
(4A) Bang SL, Belal M. AUTOLOGOUS pubovaginal SLINGS: back to the future or a lost art?. Res Rep Urol. 2016;8:11–20. (2016 Jan 18). doi:10.2147/RRU.S96957
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723033/
(4B) Isbert et al. Die Implantation von Polypropylene-Mesh induziert eine B7-2 (CD86) positive Fasciitis am Rattenmodell. [Polypropylene mesh repair for treatment of groin hernias induces a B7-2 (CD86)-positive fasciitis in rats.]
In: Menger M.D., Haas N.P., Neugebauer E., Bauer H. (eds) Chirurgisches Forum 2003 für experimentelle und klinische Forschung. Deutsche Gesellschaft für Chirurgie, vol 32. Springer, Berlin, Heidelberg.
https://link.springer.com/chapter/10.1007/978-3-642-19024-7_141#citeas
(4C) Baylón et al. Past, Present and Future of Surgical Meshes: A Review. Membranes (Basel) (22 Aug 2017);7(3):47.
doi:10.3390/membranes7030047
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618132/
(4D) Heymann et al. Polypropylene mesh implantation for hernia repair causes myeloid cell-driven persistent inflammation. JCI Insight (24 Jan 2019); 4(2): e123862. doi:10.1172/jci.insight.123862
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6413778/
(5A) Stetson, Diana. Vaginal Mesh Excision. Department of Obstetrics and Gynecology, von Voigtlander Women’s Hospital, Michigan Medicine (May 2018).
Click to access ExcisionOfMesh.pdf
(5B) Transvaginal Mesh Removal. Colorado Women’s Health, University of Colorado Hospital.
https://urogyn.coloradowomenshealth.com/patients/library/transvaginal-mesh-removal
A UK-Based Patient, Kath Sansom, Has Mesh Removal Surgery
(6A) Brown, Julia. ‘The pain was instant’: The devastating impact of vaginal mesh surgery. NewScientist (5 Sept 2018).
(6B) Sansom, Kath. Journalist Kath Sansom was ‘wreck’ after vaginal mesh implant. Sky News (30 Jan 2018).
https://news.sky.com/story/journalist-kath-sansom-was-wreck-after-vaginal-mesh-implant-11086123
(6C) Sansom, Kath. Vaginal mesh left me in agony. When will women’s health be taken seriously? The Guardian (27 April 2017).
(6D) Briggs, Caroline. Life after vaginal mesh surgery. BBC (5 April 2019).
https://www.bbc.com/news/in-pictures-47777782
A NZ-Based Patient Undergoes Several Excision Surgeries to Remove All Mesh
(7) Catie’s Story:
Real Kiwis, Real Stories. New Zealand – Mesh Down Under
http://meshdownunder.co.nz/kiwi-stories
Media – Failed Vaginal Mesh Implant Stories
Alison Blake (Suicided Following Botched Mesh Implant)
(1) McCarthy, Joanne.’There was a look in her eyes’: Mother’s emotional torment at surgery nightmare. Sydney Morning Herald (20 December 2017).
Chrissy Brajcic (Deceased At Only 42 Following Failed Mesh Implant)
(2A) McCarthy, Joanne. Canadian woman Christina Lynn Brajcic dies after receiving pelvic mesh implant. Sydney Morning Herald (4 December 2017).
Please watch 2-minute video of Chrissy’s sad surgical mesh story (now deceased at only 42 following mesh-related complications).
(2B) Marsden, Harriet. Vaginal mesh campaigner ‘dies of sepsis after antibiotic-resistant infection’. Independent (4 December 2017).
Jan Wise, A Mesh Implant Pain Sufferer
(3A) McCarthy, Joanne. Pelvic mesh victim speaks out about ‘one of the greatest medical scandals in Australian history’. The Herald (23 March 2017).
http://www.theherald.com.au/story/4547363/its-so-awful-and-so-private-photos-video/?cs=5507
Please watch 3-minute video of Jan’s tragic surgical mesh story.
(3B) McCarthy, Joanne. Pelvic mesh victim speaks out about ‘one of the greatest medical scandals in Australian history’. The Herald (23 March 2017).
https://www.theherald.com.au/story/4547363/its-so-awful-and-so-private-photos-video/
‘The Angel’ in the UK Named Dr Sohier (Suzy) Elneil, Urogynaecologist
(4A) Brown, Julia. The inside story of the vaginal mesh scandal, from top removal surgeon. NewScientist(5 Sept 2018).
(4B) Elkins, Lucy. NHS Health Heroes campaign: Surgeon who works day and night to help women told they imagined their pain. Daily Mail Australia (10 July 2018).
https://www.dailymail.co.uk/health/article-5935393/Surgeon-works-day-night-help-women-told-imagined-pain.html
Other Articles and Stories from Media
(5A) Marsden, Harriet. The biggest NHS scandal you’ve never heard of only affects women, but men should be just as concerned. Independent (5 August 2017).
(5B) Marsden, Harriet. Panorama investigation reveals medical company failed to fully inform doctors of vaginal mesh risks. Independent (11 December 2017).
(6) Moss, Rachel. What is A vaginal mesh implant? Government to launch audit into complications. Huffington Post (30/1/2018).
(7) McCarthy, Joanne. Pelvic mesh left a man ‘stabbed’ during sex, regulator warned. The Herald (17 March 2017).
http://www.theherald.com.au/story/4535453/mesh-in-stabbing-incident/?cs=5507
(8) McCarthy, Joanne. Australian pelvic mesh victims launch their case against Johnson & Johnson. The Herald (4 July 2017).
http://www.theherald.com.au/story/4769450/pelvic-mesh-victims-in-landmark-action/?cs=2452
(9) Moodie, Claire. Vaginal mesh implants: Gynaecologist urges proactive response to health concerns. ABC News (4 July 2017).
http://www.abc.net.au/news/2017-07-04/vaginal-mesh-implants-surgeon-urges-proactive-response/8677488
(10) McCarthy, Joanne. Johnson & Johnson pelvic mesh doctor said he would not want his wife to undergo procedure, Federal Court told. Sydney Morning Herald (5 July 2017).
(11) Pelvic implant lawsuit underway in Sydney. 9 News (4 July 2017).
http://www.9news.com.au/national/2017/07/04/08/57/vaginal-mesh-lawsuit-to-commence
(12) Smith, Leesa. ‘Vaginal mesh implant has destroyed my life — it’s just so hard to go on’. News (11 May 2017).
(13) For Donna’s, Catie’s, Helen’s and other mesh victim’s stories, please see:
Real Kiwis, Real Stories. New Zealand – Mesh Down Under
http://meshdownunder.co.nz/kiwi-stories
Please note: Catie’s story involving complete mesh removal may offer hope to other mesh patients.
(14A) Favaro, Avis. Woman appeals to Ottawa for temporary ban on female pelvic mesh. CTV News (8 January 2018).
(14B) Favaro, Avis & St. Philip, Elizabeth. Women with pelvic mesh complications at higher risk of depression, suicidal thoughts. CTV News (9 January 2019).
(14C) Akre, Jane. Wideman – Canadian Child Advocate and Rancher. Mesh News Desk (21/5/2012).
(14D) Welk et al. Association of Transvaginal Mesh Complications With the Risk of New-Onset Depression or Self-harm in Women With a Midurethral Sling. JAMA Surg (9 January 2019).
doi:10.1001/jamasurg.2018.4644
https://jamanetwork.com/journals/jamasurgery/article-abstract/2719817
(15) Wakatama, Giselle. Concern grows over hernia mesh as more patients share post-surgery horror stories. ABC News (14 Sep 2018).
(16) Marwick, Jane. Why aren’t we talking more about one of Australia’s greatest medical scandals? The Daily Telegraph (29 August 2017).
(17) Hooton, Amanda, & McCarthy, Joanne. The ‘eight-minute’ cure: how transvaginal mesh sentenced thousands of women to a life of pain. SMH (15 June 2019).
(18) Hennessy, Michelle. Vaginal mesh implants: Women complain of delay in aftercare for severe complications. The Journal (16/6/19).
https://www.thejournal.ie/vaginal-mesh-aftercare-4682615-Jun2019/?utm_source=shortlink
(19) Scott, Marion. Acclaimed surgeon offers to come to Scotland to ease agony of mesh victims. Sunday Post (14/1/2019).
(20) Akre, Jane. Estelle Finds Complete TVT Removal. Meshnewsdesk (12/8/2014).
https://www.meshmedicaldevicenewsdesk.com/estelle-finds-complete-tvt-removal/
(21) Left Behind by the Vaginal Mesh MDL: Survivors with Catastrophic Pain (14 July 2019).
Pelvic Mesh Support Groups
(1) Sling the Mesh – Raising awareness of the life changing risks of a “simple” day case operation
https://slingthemesh.wordpress.com/media-news-updates/
(2) Australia – Mesh Down Under
https://www.facebook.com/MeshDownUnder/
(3) New Zealand – Mesh Down Under
(4) Patient Groups: Pelvic Mesh. The Independent Medicines and Medical Devices Safety Review (Dec 2018); Pages 1 – 317.
Click to access FOR%20PUBLICATION%20Patient%20Groups%20-%20Pelvic%20Mesh.pdf
Kegel Exercises For Weak Pelvic Floor Muscles
(1) Ward, Mary. A weak pelvic floor can mean more than a little leakage. Sydney Morning Herald (18 June 2018).
Acupuncture for Stress Urinary Incontinence
(1) Kim et al. The Effect of Needle-embedding Therapy and Pharmacopuncture Therapy on Patients with Urinary Incontinence. Journal of Acupuncture and Meridian Studies (Dec 2011); 4(4): 220-4.
https://doi.org/10.1016/j.jams.2011.10.012
https://www.sciencedirect.com/science/article/pii/S2005290111000458
(2) Zhu, Angela Tian. The Million-Dollar Point. Traditional QI Energy (13 May 2011).
https://www.traditionalqi.com/2011/05/13/the-million-dollar-point-2/
In German
(1) Wenn die Vagina plötzlich zubeißt [translated: When The Vagina Suddenly Bites]. Stern (21 March 2017).