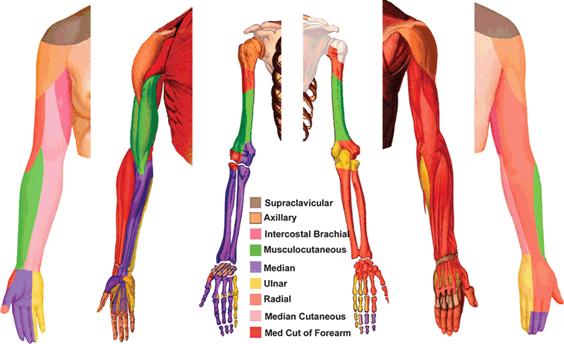
Feature Image of ‘The Innervation of the Upper Limb’
NB The roots and branches of the brachial plexus in the arm are shown below.
Source: Chelly JE, ed. Peripheral Nerve Blocks: A Color Atlas. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009: 32.
https://aneskey.com/overview-of-peripheral-nerve-blocks/
INTRODUCTION
Dear Pain Matters blog readers,
This blog post explores studies involving both children and adults with complex regional pain syndrome (CRPS) who underwent peripheral nerve blocks for pain relief.
ANATOMY OF A PERIPHERAL NERVE BLOCK
Peripheral nerve blocks are useful for diagnostic and/or therapeutic purposes.
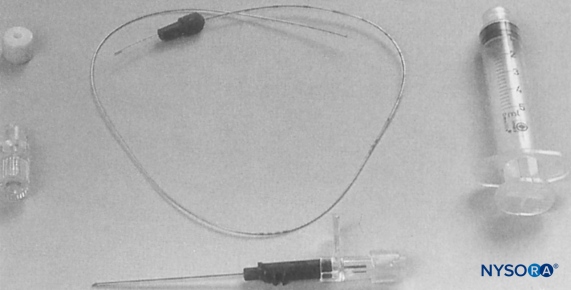
An example of a brachial plexus infusion kit used for continuous nerve block
Peripheral nerve blocks may be done either:
- Continuously via infusion pump filled with a local anaesthetic; or
- Via single injection of a local anaesthetic.
Local anaesthetics may include Bupivacaine**, Lidocaine, Mepivacaine** or Ropivacaine (Ropivacaine having less toxicity – see ‘Ropivacaine vs Bupivacaine’ section for more details).
There are many kinds of peripheral nerve blocks (e.g. upper limb blocks, lower limb blocks).
The brachial plexus is shown below. This comprises a complex network of nerves including roots and branches – some of which may targeted by a nerve block:
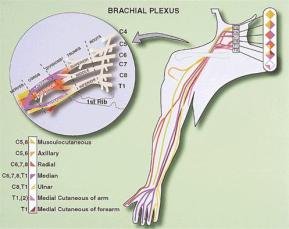
Chelly JE, ed. Peripheral Nerve Blocks: A Color Atlas. 2nd ed. Philadelphia, PA, Lippincott Williams & Wilkins; 2009: 20
https://aneskey.com/overview-of-peripheral-nerve-blocks/
The Feature Image at the top shows the innervation of the upper limb, some that may be affected by a nerve block.
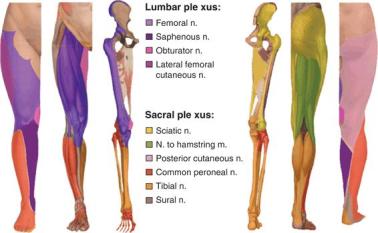
Below, the branches of the lumbar plexus (left) and sacral plexus (right) that innervate the lower limb are shown, some that may be the precise target of a nerve block:
From Chelly JE, ed. Peripheral Nerve Blocks: A Color Atlas. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009: 76 and 79.
https://aneskey.com/overview-of-peripheral-nerve-blocks/
Below, we can see the innervation of the lower limb, parts of which may be subject to a nerve block.
Chelly JE, ed. Peripheral Nerve Blocks: A Color Atlas. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009: 74
https://aneskey.com/overview-of-peripheral-nerve-blocks/
There are many videos about peripheral nerve blocks including the following 2 short videos:
(1) Peripheral Nerve Block
(2) How Nerve Blocks and Nerve Sheath Catheters Work
https://www.marshfieldclinic.org/specialties/anesthesia/anesthesiology-nerve-block
NERVE BLOCKS FOR CHILDREN WITH CRPS
(1) A French Study Shows 100% Success Including Nil Pain Following 4-Day Continuous Nerve Block for Children with CRPS (N=13)
Details of French study
Introduction
According to a French study by Dadure et al (2005), recurring or intractable CRPS1 is not rare in children.
In this study, (the lesser toxic) Ropivacaine was used for performing continuous peripheral nerve block infusions in children with CRPS1 (N=13). Ropivacaine is considered less toxic than other local anaesthetics (see ‘Ropivacaine vs Bupivacaine’ section, below).
The average age of the children was 13, with ages ranging from 9 to 16.
The VAS Pain Scores prior to 4-day continual peripheral nerve block ranged from 8 to 10. This severe nerve pain was accompanied by allodynia, numbness, swelling and vasomotor disturbances.
The inciting event(s) for CRPS1 included sprains and traumas to ankles and wrists that occurred 6 to 8 months prior to peripheral nerve block.
4-Day Continuous Peripheral Nerve Block
While under general anaesthesia, nerve block was commenced by using a nerve stimulator to precisely locate the affected nerve. Once the catheter was in place, 0.5 ml/kg of a mixture on a 1:1 basis of 0.5% Ropivacaine and 1% Lidocaine (with Epinephrine) was injected via the catheter for 5 minutes.
Thereafter, a 20-minute Bier block* that involved anaesthesia of a limb was performed. A Bier block is sometimes called intravenous regional anaesthesia.
Specifically, the Bier block that led to regional anaesthesia involved draining blood out of the limb (via exsanguination), inflating a tourniquet* and intravenously injecting a local anaesthetic (0.2 ml/kg lidocaine, 1%) and other medication.
General anaesthesia was discontinued after completion of the Bier block.
A 96-hour ambulatory continuous 0.2% Ropivacaine infusion was commenced. Twelve (12) children had popliteal nerve blocks* while the 13th child was given an axillary nerve block*.
Results
Postoperative pain relief was excellent in all 13 children with CRPS1!
VAS Pain Scores decreased from 8 – 10 to NIL following 4-day ambulatory continual peripheral nerve block in ALL 13 children with CRPS1.
Motor nerve block was minimal before 12 hours, and non-existent thereafter. All children were able to walk after 24 hours.
Early discharge from hospital and continuation of the 4-day peripheral nerve block at home was rendered possible via the use of disposable catheter pumps.
Follow-Up
All 13 children had nil pain nor other symptom of intractable or recurrent CRPS1 at the 2-month follow-up.
Summary
The authors concluded that disposable continuous peripheral nerve block with Ropivacaine infusions may be an effective treatment for recurring or intractable CRPS1.
The 4-day Ropivacaine infusion offered complete pain relief and rapid mobility. This resulted in early discharge from hospital for all 13 children with CRPS1 (Dadure et al, 2005).
A happy child is a happy life.
NERVE BLOCKS FOR ADULTS WITH CRPS
(2) A New Zealand Study – Peripheral Nerve Block for CRPS Patients (N=9)
Details
Nine (9) patients (5 females; 4 males) had severe CRPS including hyperalgesia and allodynia. The VAS Pain Scores were 9 or 10 (‘Worst Pain’) for 7 patients, and 7 or 8 (‘Severe Pain’) for the remaining 2 patients.
Many patients suffered pins and needles, tingling, numbness, redness of skin, sweating, hot or cold skin temperatures in their CRPS-affected limb as well as sleep disturbances.
The causes for CRPS varied greatly. Inciting events and injuries that led to CRPS included elbow injuries and traumas caused by crutching machine, blunt blows, a forklift blow and forceful gripping. CRPS also resulted following an injection into a thumb, a knee twisting injury, a fall onto a knee and an incident involving a hand and a 4WD door.
Treatment
These 9 CRPS patients (aged 22 to 61) were offered:
- Peripheral nerve blocks;
- Pain medications (e.g. carbamazepine, opiates); and
- Bupivacaine (Marcain) trigger point injections for myofascial pain (in some patients)
from 2002 to 2003.
Peripheral Nerve Blocks
Three ml (3ml) of Bupivacaine was injected proximal* to the site of nerve pain. This was repeated every 2 – 3 weeks (maximum 3 injections). Treatment occurred in Invercargill (N=7) and Wellington, New Zealand (N=2).
Results
Seven (7) of 9 CRPS patients enjoyed significantly less hyperalgesia and allodynia after peripheral nerve blocks and other pain treatments.
Specifically, 5 patients enjoyed NIL pain more than 1 year after discharge. Another 2 patients had VAS Pain Score reductions from 9 to 1 or 2 two years after discharge (Kanji, 2006).
Conclusion of New Zealand Study
Peripheral nerve blocks together with pain medication may be a promising pain treatment for some CRPS patients.
(3) A Dutch Study – Continuous Axillary Brachial Plexus Blockade with Bupivacaine for 6 CRPS Patients (3 Successfully Treated)
Introduction
Axillary brachial plexus blockade* was offered for patients with severe upper limb CRPS (N=6).
Specifically, an indwelling catheter was placed within the neuromuscular sheath.
Regional anaesthesia was done either:
- Continuously via portable infusion pump filled with Bupivacaine (0.5%, 3ml/hour); or alternatively,
- Via a daily single dose of 20 ml Bupivacaine (0.25%) half an hour before therapy.*
Half (N=3) of the 6 Dutch CRPS patients benefited from brachial plexus blockade.
Details of all 6 patients follow:
Patient 1 (Unsuccessful Nerve Block due to Irritation at Catheter Insertion Site)
Sadly, Patient 1 (let’s call her ‘Eliza’) did not permanently benefit from brachial plexus blockade.
Eliza was 31 when she had right hand surgery for morbus Quervain.* Following casting, Eliza’s forearm was swollen and cold. Additionally, she had persistent and intense burning pain and severe allodynia in the right arm. A diagnosis of reflex sympathetic dystrophy (RSD; now called CRPS1) was made. Conventional pain intervention did not offer any relief and her arm lost all function due to severe muscle weakness.
Eliza was offered a continuous axillary brachial plexus blockade 2 years after she was first diagnosed with RSD.
The good news:
Within only hours of the continuous axillary brachial plexus blockade, Eliza’s right arm became warm, her pain decreased and the range of motion in her RSD-affected joints almost returned to normal.
The bad news:
Sadly, due to irritation at the catheter insertion site, Eliza’s continuous axillary brachial plexus blockade was stopped. Instead, she received a daily single dose of Bupivacaine.
Despite this, all of Eliza’s severe RSD symptoms returned within weeks after her continuous axillary brachial plexus blockade was discontinued.
Patient 2 (Successful Nerve Block)
Patient 2 (let’s call her ‘Alina’) was 39 when she suffered trauma including dislocation to her left shoulder during an epileptic seizure. After her dislocated left shoulder was repositioned, Alina felt a ‘burning diffuse pain’ in her left arm that was also swollen. Despite pain medication, Alina suffered severe allodynia and continuous burning pain in her entire left arm. Her left arm remained swollen, red, warm and sweaty. Her left hand’s range of motion was severely restricted and painful.
Nerve tests via electroneuromyography showed a small left brachial plexus lesion as well as deficient motor and sensory conduction velocity in her ulnar nerve. Alina was diagnosed with RSD following three-phase bone scanning.
Despite conventional pain treatment for 2 months, Alina’s RSD symptoms did not improve.
As such, Alina was offered a daily single dose of Bupivacaine.
The good news:
After receiving her first injection of Bupivacaine, she immediately enjoyed significant pain relief, reduced swelling and enhanced mobility. Her left hand function also improved.
After completing 2 sessions, Alina’s Bupivacaine treatment were no longer necessary. Alina’s RSD symptoms were vastly improved and lasting, as indicated at the follow-up appointment more than 1 year later.
Patient 3 (Unsuccessful Nerve Block due to Infection and Abscess)
Sadly, Patient 3 (let’s call her ‘Abby’) did not permanently benefit from brachial plexus blockade.
At 41 and while carrying glass bottles, Abby accidentally fell and severed 4 extensor tendons in her right wrist. Her forearm was casted following reconstructive surgery. Almost immediately afterward, her forearm became swollen. Furthermore, it switched from being red and warm to cold and blue. The cast had to be removed due to severe allodynia and continuous burning pain.
Despite conventional pain treatment for 2 months, Abby’s severe pain and swelling persisted. There was also excess hair and nail growth as well as wasting of skin.
Abby was diagnosed with RSD following three-phase bone scanning.
The good news:
Within a few hours of the continuous axillary brachial plexus blockade, Abby’s right forearm and hand became warm with significantly less pain and swelling. Abby was finally able to undertake physiotherapy.
The bad news:
Sadly, due to local infection at the catheter insertion site that spread to an abscess below the skin, Abby’s continuous axillary brachial plexus blockade was stopped after 3 sessions.
Following discontinuation of her nerve block, Abby’s severe pain and all of her other RSD symptoms and disability returned.
Patient 4 (Successful Nerve Block)
At 52, Patient 4 (let’s call her ‘Erin’) had right hand surgery due to Dupuytren contractures.* This was following up with a second hand operation to correct hand function. Erin had severe burning pain in her entire right arm that prevented her from sleeping, performing domestic chores and playing the piano.
Four (4) months later, Erin had severe pain, reduced sensation and swelling in her right hand. She was diagnosed with RSD following three-phase bone scanning.
The good news:
Erin underwent 3 sessions of continuous axillary brachial plexus blockade, during which she was pain free and able to do physiotherapy.
Despite minor contractures in several finger joints in her right hand (that compromised her ability to play the piano), her muscle strength fully recovered.
Patient 5 (Successful Nerve Block)
At 57, Patient 5 (let’s call her ‘Janet’) underwent casting following bilateral Colles fractures.* Her right hand remained painful.
Seven (7) later, Janet was diagnosed with RSD via three-phase bone scanning.
Janet received 4 sessions of daily single dose of Bupivacaine.
The good news:
These injections led to significant pain relief and enhanced muscle strength in her right hand.
After 2 months, all of her pain had vanished and her hand function including writing ability was restored.
The same results were confirmed at her 21-month follow-up appointment.
Patient 6 (Unsuccessful Nerve Block)
Sadly, Patient 6 (let’s call her ‘Lina’) did not permanently benefit from brachial plexus blockade.
At 43, Lina had RSD in her right leg for 7 years.
More recently and for unclear reasons, her right hand became painful, warm, red and swollen. Lina was diagnosed with RSD in her right hand.
Despite 7 months of conventional pain treatment, Lina had continuous burning pain and allodynia in her right forearm that was also cold. There was skin, nail and muscle wasting as well as severe contractures in her wrist and hand joints. Functional use of her right hand was impossible.
The good news:
Lina enjoyed immediate benefits upon commencing daily single dose of Bupivacaine. Her right hand became warm and the pain was reduced. After 3 sessions of Bupivacaine injections, Lina was able to perform activities using both hands.
The bad news:
Within only weeks after stopping Bupivacaine injection treatment, Lina’s pain and other RSD symptoms returned and functional activities using her hands were no longer possible.
Conclusion of Dutch Study
Three (3) of 6 CRPS patients (50%) benefited from axillary brachial plexus blockade.
Interestingly, the remaining 3 CRPS patients temporarily benefited from brachial plexus blockade. However, as soon as continuous axillary brachial plexus blockade was stopped (either due to irritation or local infection/abscess, as in Patients 1 and 3, respectively), pain and other symptoms of RSD returned.
Instead of a continuous axillary brachial plexus blockade, the 6th patient received daily single dose Bupivacaine injections.
The authors of this Dutch study asked a very interesting question (quoting):
‘Would continuous pain reduction with continuous axillary brachial plexus blockade (BPB1) have resulted in better functional use of the affected hand in activities of daily life and thereby improve long term effect? Continuous axillary brachial plexus blockade seems more effective than daily single dose Bupivacaine injections (BPB2) in interrupting a … vicious [inserted: pain] circle and in preventing centralization and seems first choice when axillary brachial plexus blockade (BPB) is considered in treating severe RSD of an upper exteremity in which … exercises are not tolerated … Further studies are needed …’ (Ribbers et al, 1997; Ribbers, 2001).
In other words, would a better outcome have occurred if all 6 patients had continuous axillary brachial plexus blockade (assuming nil complications)?
(4) The English Patient with RSD
A 37-year old woman (let’s call her ‘Anne’) suffered neck (i.e. cervical) and shoulder pain as well as an occipital headache* following a car accident.
Six (6) weeks later, Anne endured pain in her left hand that was cold, blue, swollen and weak with reduced sensation.
Six (6) months later, Anne’s left hand was continuously painful (8/10), swollen, cold and in a semi-claw position. Following various tests, a diagnosis of RSD was made for the first time. (Unfortunately, Anne’s pregnancy had to be terminated following exposure to diagnostic tests that may have resulted in birth defects.)
Almost a year after her car accident, Anne was successfully treated with a 48-hour continuous axillary brachial plexus Bupivacaine block via a catheter inserted into her axillary sheath.
The good news:
Anne was finally free of pain during the Bupivacaine infusion! She was able to regain some movement of her hand and fingers during the next 2 weeks.
Since some of the pain in her left hand had returned, 2 more 24- to 48-hour continuous axillary brachial plexus Bupivacaine blocks were added to her care.
Six (6) hours after the infusion, Anne was (again) pain free. Furthermore, she regained a full range of movement in her left hand.
At her follow-up appointment 2 months later, Anne’s pain in her left hand was ‘minimal’ (1/10) and she continued to enjoy full movement of her left hand and fingers (Murray et al, 1995).
(5) An American Study – Continuous Infusion of Lidocaine Leads to Pain Relief in 5 CRPS Patients
Nine (9) patients with CRPS were selected for continuous subcutaneous 10% lidocaine infusion treatment. Four (4) patients had to discontinue this treatment.
Of the 5 who actually completed this treatment for 4 – 8 weeks, 4 were female (average age 47) while 1 was male. All 5 were diagnosed with CRPS 2.5 to 8 years earlier before commencing this treatment.
Post-continuous lidocaine infusion treatment , all 5 CRPS patients enjoyed less pain and allodynia. Their VAS Pain Scores decreased from 7 – 10 to 2 – 5.
There were also improvements in other CRPS symptoms (Linchitz & Raheb, 1999).
(6) A CRPS Patient in Saudi Arabia: Single Injection Nerve Block for CRPS
A 34-year old female patient (let’s call her ‘Azza’) suffered severe pain and allodynia (9 – 10 out of 10) in her left hand and wrist that was swollen, pale, cool, clammy, numb and weak. Azza also had limited movement in her left shoulder. Azza’s symptoms started 5 months ago although she could not remember any cause.
A diagnosis of CRPS1 was made.
Azza received an ultrasound-guided nerve block (i.e. interscalene brachial plexus block*). This nerve block that involved a single injection shot of 30ml Bupivacaine 0.25% resulted in complete pain relief in her left hand within a week.
Azza was also given a trigger point injection for spasms in her trapezius muscle that caused neck pain. At first, the trigger point injection involved lidocaine 2% infiltration. Two weeks later, Azza was offered another trigger point injection using botulinum toxin (BTX-A 100u; Botox) that finally led to lasting pain relief in myofascial trigger points in her trapezius muscle in her shoulder.
Azza’s functional mobility was restored via physiotherapy.
In summary and as confirmed at her 3-month follow-up, Azza enjoyed 100% pain relief from CRPS1, left hand, and full limb mobility following a single interscalene injection using Bupivacaine.
Azza’s neck pain caused by trapezius muscle spasms was completely resolved by a myofascial trigger point injection using Botox (Fallatah, 2014).
(7) Ulnar Nerve Block for RSD
A patient was diagnosed with upper limb RSD following radiography of blood vessels in the brain via the subclavian artery*. To enhance imaging, contrast injections are necessary.
Using a stimulator to identify the ulnar nerve in the axillary bundle, low volume injections including Bupivacaine 0.5% were given.
These injections led to pain relief and reversal of other RSD symptoms (Klein & Klein, 1991).
(8) A Slovenian Study Involving Continuous Sensory Analgesia for CRPS, Upper Limb
This review explores 21 CRPS patients who were screened for treatment involving continuous sensory analgesia via brachial plexus blockade.
In the first 2 days, all 21 patients underwent non-invasive therapy that included elevation of the CRPS-affected limb, cryotherapy and active exercises. Cryotherapy involves placing ice and cold packs near a painful area to reduce inflammation and soothe pain.
While 5 patients benefited from this non-interventional treatment, 16 did not.
As such, these 16 CRPS patient had continuous sensory analgesia of brachial plexus. This nerve block was done within 1 to 6 months after the inciting injury.
Patients were followed up from 3 months to 3 years after continuous sensory analgesia. Two (2) patients enjoyed excellent results (i.e. a completely normal hand), 11 patients had good results while 3 had poor results (Margić & Pirc (2003).
ROPIVACAINE vs BUPIVACAINE
Toxicity of Bupivacaine to Muscle Cells
Ropivacaine is a less potent local anaesthetic with an improved safety profile including lower muscle toxicity compared to Bupivacaine (Kaur et al, 2015).
An animal study found that Bupivacaine was toxic to muscle cells, especially in young rats.
Specifically, Bupivacaine led to bioenergetic alterations within the mitochondria* in muscle cells. This led to severe abnormalities in the muscle ultrastructure including damaged sarcomeres inside the muscle cells themselves (Nouette-Gaulain et al, 2009).
Selectivity of Ropivacaine for Sensory Nerves – Not Motor Nerves
Furthermore, at lower concentrations, motor nerves may remain unaffected throughout a Ropivacaine blockade (compared to Bupivacaine that initially blocks both sensory and motor nerves). This is due to the selectivity of Ropivacaine blockade for sensory nerves only.
Thus, reduced or nil pain sensation and unaffected motor nerves following a sensory nerve block with Ropivacaine may facilitate physiotherapy (Markham & Faulds, 1996).
SUMMARY
In summary, peripheral nerve blocks (together with other pain treatments) may offer significant relief from pain and other symptoms of CRPS.
This can only be good news!!
Sabina Walker
Blogger, Pain Matters (in WordPress)
KEY
* Mitochondria are the cells’ powerhouse or engine room and even have their own DNA.
* Sarcomeres are the ‘building blocks’ of our skeletal muscle cells.
* An axillary brachial plexus block (or axillary nerve block) is a nerve block for the lower arm (i.e. forearm) including elbow, wrist and hand.
An axillary corresponds to an armpit or part thereof.
Brachial pertains to the arm or part thereof.
* Exsanguination forces blood out of the limb, or part thereof. The use of an inflatable tourniquet prevents the return of blood flow into this area until desired.
* In a Bier block, a tourniquet is used to restrict local anaesthetic to a certain limb area and hence prevent it from entering circulation.
* A popliteal nerve block is a distal sciatic nerve block that leads to anaesthesia of the lower leg including calf, tibia, fibula, ankle, and foot.
Distal means further from the centre of the body.
* Proximal means closer to the centre of the body (e.g. spinal cord).
* Morbus Quervain, or de Quervain syndrome, involves pain and inflammation in the thumb including its tendons.
* Dupuytren’s contracture involves knots of tissue that form under the skin of the palm of a hand that leads to a deformed hand.
* A Colles fracture is a distal forearm fracture (ie broken wrist).
* Occipital headache may be caused by injury to head, neck and upper cervical spine that adversely affects the occipital nerves.
* An interscalene brachial plexus block is a proximal block of the brachial plexus.
* The subclavian artery delivers oxygenated blood from the base of the neck to the brain.
* Bupivacaine treatment was offered for a maximum of 2 weeks, followed by a 1-week ‘rest’ period. This was done to prevent infection, scar tissue and fibrosis as well as other complications at the catheter insertion and/or injection site. These 3-week cycles (aka sessions) were repeated as necessary.
** The local anesthetic, Mepivacaine, preferentially blocks sodium channel Nav1.8, while Bupivacaine inhibits TTX-sensitive sodium channels (Leffler et al, 2010).
REFERENCES
NERVE BLOCKS FOR CHILDREN WITH CRPS
(1) Dadure et al. Continuous Peripheral Nerve Blocks at Home for Treatment of Recurrent Complex Regional Pain Syndrome I in Children. Anesthesiology (Feb 2005);102(2):387–91.
NERVE BLOCKS FOR ADULTS WITH CRPS
(2) Kanji, Giresh. Treatment of Complex Regional Pain Syndrome with Peripheral Nerve Blocks: A Case Series of Nine Patients. Australasian Musculskeletal Medicine (June 2006); pages 1-10.
https://rsds.org/wp-content/uploads/2015/02/Kanji_2010.pdf
(3A) Ribbers et al. Axillary brachial plexus blockade for the reflex sympathetic dystrophy syndrome. International Journal of Rehabilitation Research (1997); 20; 371-380.
https://www.ncbi.nlm.nih.gov/pubmed/9459103
(3B) The above Dutch paper also forms part of this 150-page thesis paper:
Ribbers, Gerardus Maria. Complex Regional Pain Syndrome I – A Study on Pain and Motor Impairments (2001); Go to Chapter 5, pages 69 to 84.
ISBN: 90-74443-33-8
https://repub.eur.nl/pub/23547/011024_Ribbers,%20Gerardus%20Maria.pdf
(4) Murray et al. Continuous axillary brachial plexus blockade for reflex sympathetic dystrophy. Anaesth 1995;50:633-5.
https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1365-2044.1995.tb15117.x
(5A) Linchitz RM & Raheb JC. Subcutaneous Infusion of Lidocaine Provides Effective Pain Relief for CRPS Patients. The Clinical Journal of Pain (1999); 15: 67-72.
https://www.ncbi.nlm.nih.gov/pubmed/10206569
(5B) Martin, Craig. Subcutaneous Lidocaine Infusion as Treatment for Complex Regional Pain Syndrome (CRPS). WorkSafeBC (October 2016); Pages 1-5.
(6) Fallatah, Summayah MA. Successful management of complex regional pain syndrome type 1 using single injection interscalene brachial plexus block. Saudi J Anaesth (Oct-Dec 2014); 8(4): 559–561.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4236948/#__ffn_sectitle
(8) Margić & Pirc. The treatment of complex regional pain syndrome (CRPS) involving upper extremity with continuous sensory analgesia. European Journal of Pain (2003); 7(1):
https://doi.org/10.1016/S1090-3801(02)00052-6
https://onlinelibrary.wiley.com/doi/abs/10.1016/S1090-3801%2802%2900052-6
ROPIVACAINE, BUPIVACAINE and Mepivacaine
(9) Nouette-Gaulain et al. Age-dependent bupivacaine-induced muscle toxicity during continuous peripheral nerve block in rats. Anesthesiology (Nov 2009);111(5):1120-7.
doi: 10.1097/ALN.0b013e3181bbc949
(10) Kaur et al. Comparision between bupivacaine and ropivacaine in patients undergoing forearm surgeries under axillary brachial plexus block: a prospective randomized study. J Clin Diagn Res (2015);9(1):UC01-6.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4347153/pdf/jcdr-9-UC01.pdf
(11) Markham A & Faulds D. Ropivacaine. A review of its pharmacology and therapeutic use in regional anaesthesia. Drugs (1996); 52: 429–49.
https://www.ncbi.nlm.nih.gov/pubmed/8875132
(12) Leffler et al. Block of sensory neuronal Na+ channels by the secreolytic ambroxol is associated with an interaction with local anesthetic binding sites. Eur J Pharmacol (2010); 630:19–28.
doi: 10.1016/j.ejphar.2009.12.027