Category Archives: Chronic Pain
Eric Clapton, Musician, and his Covid Vaccine Injury – Safe and Effective?
Source of Featured Image
“… ramped up from, on a scale of ten, say, from 3 to … 8 or 9 … Agony and chronic pain …”
(Go to 10:20 minutes for screenshot.)
Please note: The advertisements are NOT mine.
Dear Pain Matters readers,
Sadly, countless people suffer from severe adverse reactions including chronic pain following their experimental Covid mRNA injections including famous musician, Eric Clapton.
Quoting Eric Clapton in an interview with Robin Monotti, Italian architect and film producer, regarding his adverse reaction to the AstraZeneca injection:
“I can’t sleep because of the pain … the vaccine took my immune system and just shook it around …
… and I went and had the jab and I got a little green [card] (like a library card), and I thought that’s what I’m going to show the people when I get on the plane. … Within several hours, I was shaking like a leaf and I went to bed early and I couldn’t get warm … I thought … am I running a fever? I was boiling hot and sweating, and then I was cold. … I was out for the count for about a week.
I had been preparing for a project where I was going to be playing acoustic guitar with a couple of musicians and we were going to film it that week. Knocked me out and I had to start again from scratch. … It didn’t come off as well as I would like to … It was a huge setback and it frightened the **** out of me because I didn’t know how long it would last. I then started to find out more …
… bit by bit, I realised that I probably shouldn’t have had the first jab but then I was offered the second [jab]. I thought, well, … what’s the point in … stopping now? So I went and had the second [jab], … And then it got really bad and within about a week, I had lost my hands – [they] didn’t really work. … I suffered from a condition … called peripheral neuropathy, which is nerve damage pain, … which means that … I can get numb, or pins and needles. …
This [pain] … ramped up from, say, 3 to … 8 or 9 (on a scale of 10). Agony and chronic pain … I have gigs to do, I have recording work to do, but I can’t … play the guitar, it’s not fun and it’s something I do … then when I put [the guitar] down, [the pain] is there until I go to bed. I take sleeping pills because I can’t sleep because of the pain, and that’s … not a good way to live … the vaccine took my immune system and just shook it around again, and that’s still going on …
… and I called my … NHS doctor after the second jab and I said, “I’ve been told there’s a yellow card system … where I can complain about after-effects?“ He said … , “I’ll fill in the report …” …
I lost the use of my hands for about 3 weeks, so I thought I was in real trouble. That’s about that point I was invited by Robin Monotti to talk about it … because I realised that … I wasn’t the only one that was suffering adverse reactions … I can’t touch anything cold or hot, I have to use these [gloves], otherwise my hands will begin to burn and they’ll stay burnt all day.
… that’s my experience from having had the second jab … I went to my doctor … and said, you know, I can’t have any more vaccinations. This is not possible for me because I don’t know what will happen. I don’t know what will happen next. …”
Source:
Eric Clapton: Exclusive & Uncensored Oracle Films – Robin Monotti in conversation with Eric Clapton
(24 minutes; transcript available; 14 June 2021; 492,000 views)
https://www.youtube.com/watch?v=4OHmMKrVbNk
via https://t.me/robinmg/26449
Quoting Eric Clapton in another interview with Robin Monotti:
“In February [2021] this year, before I learned about the nature of the [Covid] vaccines and being 76 with emphysema, I was in the avant garde. I took the first jab of [AstraZeneca] and straight away, [I] had severe reactions which lasted 10 days, I recovered eventually and was told it would be 12 weeks before the second one…
About 6 weeks later, I was offered and took the second [AstraZeneca] shot, but with a little more knowledge of the dangers. Needless to say, the reactions were disastrous. My hands and feet were either frozen, numb or burning, and pretty much useless for 2 weeks. I feared I would never play again. I suffer with peripheral neuropathy and [I] should never have gone near the needle. But the propaganda said the vaccine was safe for everyone. …”
Source:
Robin Monotti: A Conversation with Eric Clapton | Oracle Films
(22-minutes; transcript available; 16 June 2021)
via https://t.me/robinmg/3377,
Thank you very much, Robin Monotti, for sharing Eric Clapton‘s experiences that will hopefully help others struggling with side effects including chronic pain, post-Covid injection.
In closing today, I leave you with 2 songs by Eric Clapton, one written in 2021 and the second one written in 1992. Like so many of his songs, the lyrics to these songs are laden with meaning hence worthwhile analysing in greater detail:
This Has Gotta Stop
…
I knew that somethin’ was goin’ on wrong
When you started layin’ down the law
I can’t move my hands, I break out in sweat
I wanna cry, can’t take it anymore
…
I’ve been around long, long time
Seen it all, and I’m used to being FREE
I know who I am, try to do what’s right
So lock me up and throw away the key
This has gotta stop
Enough is enough
I can’t take this BS any longer
It’s gone far enough
If you wanna claim my soul
You’ll have to come and break down this door
Tears In Heaven
https://www.youtube.com/watch?v=JxPj3GAYYZ0
Sabina Walker
Master in Applied Science (Neuroscience)
Blogger, Pain Matters
ADDITIONAL REFERENCES
(1) Eric Clapton: I should never have gone near the needle.
(3) Makis, William MD
Musicians Injured – Eric Clapton: “I can’t sleep because of the pain … the vaccine took my immune system and just shook it around” –
Eric Clapton bravely discusses his neurological COVID-19 vaccine injuries (11 February 2023)
https://makismd.substack.com/p/eric-clapton-i-cant-sleep-because
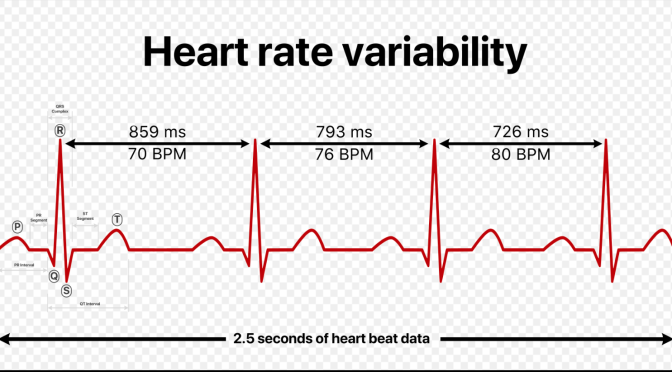
Researchers in Oslo, Norway, Explore the Relationship Between Heart Rate Variability (HRV) and Pain
Source of Featured Image
https://en.wikipedia.org/wiki/Heart_rate_variability
Dear Pain Matters readers,
Renowned heart rate variability (HRV) researchers, Associate Professor Daniel Quintana, PhD candidate Emilie Kildal and colleagues in Oslo, Norway, have recently written a science paper (not yet formally published) called:
Heart Rate Variability and Pain: A Protocol for a Systematic Review and Meta-Analysis (August 2023)
Why is this exciting?
Heart rate variability including heart rate variability – high frequency (HRV-HF) may add further objective insight into patients’ pain intensities, in addition to current diagnostic tools (that often involve subjective diagnostic tools such as pain questionnaires). For example, many patients including nonverbal patients (e.g. dementia), babies/toddlers and those with language difficulties (e.g. recent migrants) may not be able to comprehend the pain questionnaires.
Quoting from the draft science paper by Kildal, Quintana and colleagues,
“Establishing a reliable pain biomarker may significantly improve care for nonverbal patients otherwise unable to express their pain (e.g., individuals with profound autism, cerebral palsy, aphasia due to stroke, or profound intellectual disability). Amidst potential candidates, heart rate variability (HRV) has garnered growing attention. … … we aim to elucidate the association between HRV and pain. …”
Thus, Quintana and colleagues aim to explore:
– the relationship between HRV and experimentally induced pain;
and
- how chronic pain patients compare to healthy individuals with respect to HRV.
We eagerly await the findings of this Systematic Review and Meta-Analysis planned by the team headed by Daniel Quintana at the University of Oslo, Norway.
See my 2 other blog posts on HRV including why and how HRV could offer another (more objective) way to diagnose pain:
1)
2)
Sabina Walker
Blogger, Pain Matters
REFERENCES
(1) Kildal, E.S.M., … Quintana, D.S. Heart Rate Variability and Pain: A Protocol for a Systematic Review and Meta-Analysis (16 August 2023)
(2) Kildal, E.S.M., Quintana, D.S., Szabo, A. et al. Heart rate monitoring to detect acute pain in non-verbal patients: a study protocol for a randomized controlled clinical trial. BMC Psychiatry 23, 252 (2023). https://doi.org/10.1186/s12888-023-04757-1
‘Off-Label’ Use of Epidiolex (Cannabidiol; CBD) and Tilray 2:100 for Pain?
Feature Image of Epidiolex (cannabidiol; CBD) bottles sourced from:
Dear Pain Matters readers,
Epidiolex (Cannabidiol; CBD)
Overview
An oral solution called Epidiolex (cannabidiol; CBD) was approved on 25 June 2018 by the US Food and Drug Administration (FDA). Made by GW Pharmaceuticals, Epidiolex may be used for the treatment of epileptic seizures in patients with Lennox-Gastaut syndrome and Dravet syndrome aged 2 and above.
Epidiolex is the first FDA-approved drug that is based on a molecule (i.e. CBD) derived from marijuana (in this instance, CBD-rich cannabis). Contrary to tetrahydrocannabinol (THC) that may lead to a ‘high’, the CBD molecule does not exert psychoactive effects.
For more information about CBD and pain, please visit my blog post called:
Cannabidiol (CBD) – ‘Cannabis With the Fun Bit Taken Out’ – For Severe Chronic Pain
Possible ‘Off-Label’ Use of Epidiolex (Cannabidiol; CBD) for Pain
Given that:
- Cannabidiol (CBD) may offer pain relief; and
- Epidiolex virtually is CBD,
‘off-label’ use of Epidiolex for pain may be warranted (Anson, 2018; Urits et al, 2019).
Thus, while specifically approved for the treatment of certain epileptic conditions, ‘off-label’ prescription by doctors for Epidiolex for pain may be possible.
Tilray 2:100
Tilray 2:100 (that is comparable to Epidiolex) is now available in Canada for patients with epilepsy. Tilray 2:100 offers a target concentration of 100 mg/ml of CBD and 2 mg/ml of THC (Henriques, 2019; Tilray, 2018).
Similar to Epidiolex, ‘off-label’ prescription by doctors for Tilray 2:100 for pain may be warranted.
Summary
You may ask yourself,
‘Why would anyone request an ‘off-label’ prescription for Epidiolex or Tilray 2:100 when one could simply buy CBD for pain online (where legal)?’
According to Kyle Varner, MD, Internal Medicine Specialist in Washington:
‘CBD oil has tremendous therapeutic potential. Epidiolex is just CBD— but sold at a price tag of over $30,000 per year’ (Tapp, 2019).
The answer is that many CBD products sold online are mislabeled and unregulated. This may lead to ineffective treatments and/or side effects (Bonn-Miller et al, 2017).
As such, Epidiolex and Tilray 2:100 may be prescribed ‘off-label’ for pain in the US and Canada, respectively (in addition to, or instead of, CBD).
This is great news! Now there are more treatment options available for pain!
Please forward to anyone who may benefit from this blog post.
Sabina Walker
Blogger, Pain Matters (in WordPress)
REFERENCES
Epidiolex
(1) Urits et al. An Update of Current Cannabis-Based Pharmaceuticals in Pain Medicine. Pain Ther (5 Feb 2019).
doi: 10.1007/s40122-019-0114-4.
https://www.ncbi.nlm.nih.gov/pubmed/30721403
(2) Anson, Pat. FDA Approves First Marijuana-Based Prescription Drug. Pain News Network (25 June 2018).
(3) van der Walt, Eddie & Dawson, Rob.America’s First Cannabis-Based Medicine Is Made in England. Bloomberg (31
(4) FDA. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. FDA (25 June 2018).
https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm611046.htm
(5) Tapp, Fiona. Businesses envision a boom in CBD, the non-intoxicating oil from hemp. Boston Globe (24 Jan 2019).
Tilray 2:100
(1A) Henriques, Carolina. Tilray Launches New High-CBD Cannabis Oil for Seizure Treatment in Canada. Dravet Syndrome News (29 May 2019).
(1B) Tilray Introduces New High-CBD Extract. Tilray (06/19/2018).
https://www.tilray.ca/en/blog/post/tilray-introduces-new-high-cbd-extract/
Labelling Accuracy of Cannabidiol Available Online
(1A) University of Pennsylvania School of Medicine. Nearly 70 percent of cannabidiol extracts sold online are mislabeled, study shows. Science Daily (7 Nov 2017).
https://www.sciencedaily.com/releases/2017/11/171107112244.htm
(1B) Royal Queen Seeds. The Recent Approval of Epidiolex and its Implications.
https://www.royalqueenseeds.com/blog-the-recent-approval-of-epidiolex-and-its-implications-n1014
(1C) Bonn-Miller et al. Labeling Accuracy of Cannabidiol Extracts Sold Online. JAMA (2017); 318(17): 1708.
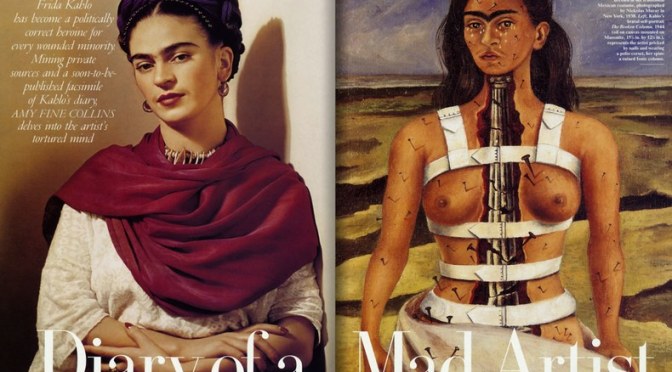
Frida Kahlo, the Mexican Heroine of Pain (La Heroina del Dolor)
This Feature Image depicts the beautiful and talented painter, Frida Kahlo (on left). It also shows one of Frida’s famous paintings called ‘The Broken Column’ that embodies her own severe pain and suffering (on right).
Feature Image sourced from:
https://www.vanityfair.com/culture/1995/09/frida-kahlo-diego-rivera-art-diary
INTRODUCTION – FRIDA KAHLO (1907 – 1954)
Dear Pain Matters blog readers,
I was first ‘introduced’ to the famous Mexican artist, Frida Kahlo, by my own beautiful daughter, Sarah, who invited me to watch the movie ‘Frida’ with her.
Diminutive in stature, Frida was larger than life itself.
Known for her talent as a Surrealist painter, Frida is a beloved cultural icon in Mexico.
Sadly, Frida endured a spate of tragedies that resulted in lifelong chronic pain including excruciating back pain.
Born to a German father and a mestiza* mother on 6 July 1907, Frida was stricken with polio when she was about 6. Polio caused her right leg and foot to be severely damaged and left her with a permanent limp.
Sadly, polio was not the only tragedy in Frida’s life.
Quoting Frida:
‘I suffered two grave accidents in my life. One involved a bus, the other is [husband] Diego.’
FRIDA’S FIRST GRAVE ACCIDENT – THE BUS CRASH
In addition to polio, tragedy struck on 17 September 1925 when Frida was only 18. While returning home from Mexico City with her then-boyfriend, the wooden bus that they were travelling in crashed into a tram.
During this bus accident that involved multiple fatalities, a steel handrail smashed Frida’s pelvis and was impaled through her left hip, belly and womb, exiting through her genitals.
Needless to say, Frida’s injuries were severe and horrific and included fractures in her back, collarbone and two ribs. Her lower spine and pelvis were both broken in 3 different places while her left shoulder was out of joint. Frida’s polio-deformed right leg had eleven (11!) fractures and her right foot was dislocated and crushed (Rogers, 2009). (Wow! Imagine going through all that!!)
Amazed that Frida barely survived this terrible bus accident, doctors (correctly) predicted that she would never have children.
Instead, chronic pain would become her ultimate companion.
To distract herself from the boredom of 2 years of bed rest including months in a plaster corset to hold her body in place, Frida started to paint extensively and with great passion.
It was at this stage in her life when Frida decided to become a painter instead of a doctor.
FRIDA’S SECOND ‘GRAVE ACCIDENT’ – HER VOLATILE MARRIAGE WITH FAMOUS ARTIST, DIEGO RIVERA
On 21 August 1929, Frida married Diego Rivera, a chronic cheater during his previous relationships. At 42, Diego was 20 years older than Frida, overweight and very big. Diego was also a well-travelled and famous painter whose friends included Pablo Picasso, Amedeo Modigliani and Leon Trotsky.

Wedding photo of Frida and Diego
Source of Image:
Pinterest and https://www.watson.ch/wissen/frauen%20der%20geschichte/407183389-frida-kahlo-die-frau-die-den-tod-auslachte
Whilst in love, their relationship was a turbulent one that included a year-long divorce. Diego continued with his many extramarital affairs.
Deciding to ‘fight fire with fire’, Frida indulged in her own extramarital affairs (including an affair with her husband’s friend, Leon Trotsky) while also exploring intimacy and sexuality with other women.
While trying to have a baby with Diego, Frida had to abort a pregnancy because of health issues pertaining to her bus crash in 1925. She also suffered a miscarriage in 1932 (Espinoza, 2007).
(Whilst it would be interesting to explore Frida’s vivacious and colourful love life, this is outside the scope of this blog. See references below including Lisa Waller Rogers for further details.)
FRIDA’S CHRONIC PAIN INCLUDING SEVERE BACK PAIN
Frida endured more than 30 operations after her severe bus accident until her death in 1954. This included 7 spinal operations, one that involved a 2nd spinal fusion because the wrong vertebrae were fused during an earlier operation. Frida also had her right leg amputated (see below).
Frida’s increasing pain levels meant that she could only paint for short periods of time.
Frida’s health issues only worsened with time. Her rigid medical corset no longer supported her failing spine and she had to undergo radical spinal and leg surgery.
In 1953, her right leg had to be amputated below her knee due to gangrene that may have resulted from a previous surgery.
Sadly, Frida, the Mexican Heroine of Pain (La Heroina del Dolor), died on 13 July 1954, having turned 47 only one week earlier.
TWO PAINTINGS BY FRIDA – ‘THE BROKEN COLUMN’ AND ‘TREE OF HOPE’
‘The Broken Column’ (1944)
When looking at her painting, ‘The Broken Column’ (shown earlier and below), people often assumed that Frida was a Surrealist painter. In actual fact, Frida expressed her own reality that included severe pain in the ‘The Broken Column’.
In her words,
‘They thought I was a Surrealist, but I wasn’t. I never painted dreams. I painted my own reality.’
‘My painting carries with it the message of pain.’
Thus, Frida used her painting, The Broken Column’, to express her own excruciating pain and suffering.
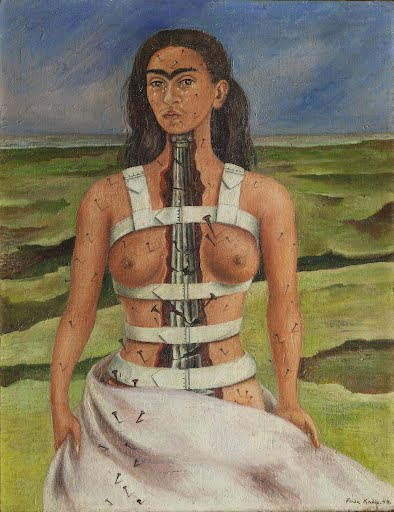
‘The Broken Column’ (Frida Kahlo, 1944)
Source of Image:
http://www.people.vcu.edu/~djbromle/artviewsnet/2002/students2002/kahlo/PetersKahlo.htm
As seen here, repeated spinal surgery had confined her body in a rigid corset apparatus. Despite holding her broken body together, her corset appears very tight, uncomfortable and restrictive.
Frida’s spinal column appears to be cracked, broken and injured in many places.
The nails embedded throughout her body clearly show the severity of her pain and suffering.
Frida shows herself as being alone in a barren wasteland. This further adds to a sense of hopelessness, helplessness, emptiness and despair.
Despite all her pain, suffering, sadness and vulnerability, Frida exudes beauty, elegance, femininity and dignity in ‘The Broken Column’ (Peters, 2002).
‘Tree of Hope’ (1946)

‘Tree of Hope’ (Frida Kahlo, 1946)
Source of Image:
https://www.fridakahlo.org/tree-of-hope.jsp
Despite bed rest and wearing a steel corset for 8 months following yet another spinal surgery, Frida’s health issues including sharp pains in her back became worse.
In response to her severe back pain and deteriorating health, Frida painted the ‘Tree of Life’.
Although Frida is seen weeping in this painting, she is hopeful for a recovery from her recent spinal operation. The Spanish words ‘Cielito Lindo’ (‘Tree of Hope, keep strong’) appear on a flag in her right hand. This flag has a red tip that looks like a surgical instrument stained with blood. Frida holds a pink orthopaedic corset in her left hand.
Frida is also seen under anaesthetic in hospital and bleeding from fresh surgical wounds following her spinal operation.
In the background, the landscape looks forlorn and barren without a trace of hope. There are 2 large fissures in the dry earth that mirror the 2 gaping wounds in Frida’s back.
Quoting Frida, this painting was ‘nothing but the result of the damned operation!’
SUMMARY
Frida leaves behind a legacy of her paintings despite suffering, and perhaps because she suffered, from chronic pain during most of her life.
I hope that you find Frida’s story inspirational, in particular, her passion for art, life and love despite enduring severe and debilitating chronic pain.
Sabina Walker
Blogger, Pain Matters (in WordPress)
* A mestiza is a person with indigenous and European ancestry.
REFERENCES
Peer-Reviewed Articles
(1) Courtney, Carol A et al; Frida Kahlo: Portrait of Chronic Pain. Physical Therapy (1 January 2017); 97(1): 90–96.
doi: 10.2522/ptj.20160036
https://academic.oup.com/ptj/article/97/1/90/2896952
https://www.ncbi.nlm.nih.gov/pubmed/27562644
(2) Antelo, Fernando. Images of Healing and Learning- Pain and the Paintbrush: The Life and Art of Frida Kahlo. American Medical Association Journal of Ethics – Virtual Mentor(May 2013); 15(5): 460-465.
doi 10.1001/virtualmentor.2013.15.5.imhl1-1305
https://www.ncbi.nlm.nih.gov/pubmed/23680570
https://journalofethics.ama-assn.org/sites/journalofethics.ama-assn.org/files/2018-06/imhl1-1305.pdf
https://journalofethics.ama-assn.org/article/pain-and-paintbrush-life-and-art-frida-kahlo/2013-05
Media, Blogs and Newspaper Articles
(1) Courtney, Carol A. Frida Kahlo’s life of chronic pain.
https://blog.oup.com/2017/01/frida-kahlos-life-of-chronic-pain/
(2) Espinoza, Javier. Frida Kahlo’s last secret finally revealed. The Guardian – Australia Edition (12 August 2007).
https://www.theguardian.com/world/2007/aug/12/artnews.art
(3) Walter, Natasha. Feel my pain. The Guardian – Australia Edition (21 May 2005).
(4) Sykes, Alan. Frida Kahlo and Diego Rivera at the Bowes Museum. The Guardian – Australia Edition (11 May 2012).
(5A) Frida Kahlo and Diego Rivera – Love and Pain. Art Gallery of NSW (25 Jun – 23 Oct 2016).
https://www.artgallery.nsw.gov.au/artboards/frida-kahlo-diego-rivera/love-and-pain/
(5B) Verghis, Sharon. Frida Kahlo: artistic genius and queen of pain. The Weekend Australian (18 June 2016).
(6) Mantalvanos, Soula. Frida Kahlo: Portrait of Chronic Pain. Pudental Nerve – Soula’s Chronic Pelvic Pain Story (25 August 2016).
https://pudendalnerve.com.au/2018/06/09/frida-kahlo-portrait-of-chronic-pain/
(7) neurophilosophy. Frida Kahlo’s life of pain. Science Blogs(24 January 2008).
https://scienceblogs.com/neurophilosophy/2008/01/24/frida-kahlos-life-of-pain
(8) Siqueira-Batista, Rodrigo et al.Art and pain in Frida Kahlo. Rev. dor – São Paulo (April/June 2014); 15(2).
http://dx.doi.org/10.5935/1806-0013.20140018
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-00132014000200139
(9) Peters, Katie. Frida Kahlo’s Self-Portraits – The Broken Column (1944). Virginia Commonwealth University(2002).
http://www.people.vcu.edu/~djbromle/artviewsnet/2002/students2002/kahlo/PetersKahlo.htm
(10) Kelley, Wes. The Painful Life of Frida Kahlo: How Injury Led to Inspiration.
Medium(14 Oct 2016).
(11) Medrut, Flavia. 17 Frida Kahlo Quotes to Inspire You to Turn Pain Into Beauty. Goalcast (28 November 2017).
https://www.goalcast.com/2017/11/28/17-frida-kahlo-quotes/
(12) Exploring Frida Kahlo’s Relationship With Her Body
https://artsandculture.google.com/theme/EQICSfueb1ivJQ
(13) Brown, Amy. Frida Kahlo – An Amazing Woman (1907-1954)
(14) Collins, Amy Fine. Diary Of A Mad Artist. Vanity Fair (3 Sept 2013).
https://www.vanityfair.com/culture/1995/09/frida-kahlo-diego-rivera-art-diary
(15) Frida Kahlo
https://en.wikipedia.org/wiki/Frida_Kahlo
(16) Frida Kahlo Corporation
https://fridakahlocorporation.com
(17) Frida Kahlo – Paintings, Biography, Quotes
https://www.fridakahlo.org/tree-of-hope.jsp
(18) Katz, Neil. Frida Kahlo Biography: Medical Mystery, Controversial Death. CBS News (6 July 2010).
https://www.cbsnews.com/news/frida-kahlo-biography-medical-mystery-controversial-death/
(19) Rogers, Lisa Waller. Lisa’s History Room – Where the Past is Always Present (26/27 May 2009).
Frida’s First Bad Accident.
https://lisawallerrogers.com/2009/05/26/frida-kahlos-first-bad-accident/
Frida Kahlo’s Other Accident.
https://lisawallerrogers.com/2009/05/27/frida-kahlos-other-accident/
Frida Kahlo: A Few Small Nips.
https://lisawallerrogers.com/2009/05/27/frida-kahlo-a-few-small-nips/
Many other fascinating blog posts by Lisa Waller Rogers are offered here:
https://lisawallerrogers.com/?s=frida+kahlo
https://lisawallerrogers.com/page/2/?s=frida+kahlo
https://lisawallerrogers.com/2009/06/10/fridas-red-hot-lover/
Films
(1A) Frida. A Hollywood production by Miramax directed by Julie Taymor (2002; 123 minutes).
https://www.miramax.com/movie/frida/
(1B) Frida, Naturaleza Viva. A Mexican film directed by Paul Leduc (1983).
Cartoons
(1) La heroine del dolor (heroine of pain).
https://zenpencils.com/comic/fridakahlo/
Article in German
(1) Rothenfluh, Anna. Frida Kahlo: Die Frau, die den Tod auslachte. Watson (14 Jan 2018).
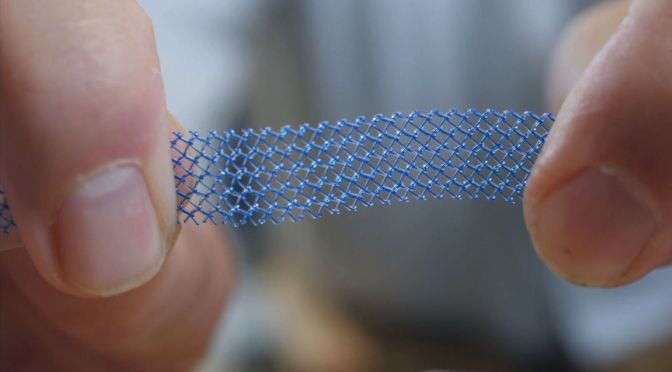
‘The Biggest Health Scandal Affecting Women Since Thalidomide’ – Can Surgery to Remove Vaginal Mesh Reduce Severe Pain Following Failed Mesh Implants?
Feature Image of vaginal mesh sourced from:
https://news.sky.com/story/journalist-kath-sansom-was-wreck-after-vaginal-mesh-implant-11086123
Dear Pain Matters blog readers,
This blog post aims to offer hope, inspiration and courage to those women who suffer from severe and ongoing pelvic pain due to failed vaginal mesh implant surgery.
Pelvic mesh implant surgery was often recommended when conservative treatments for prolapse, incontinence and other pelvic conditions failed.

Source: Stocktrek images via Getty Images
Many women were ill-advised of the high risks associated with mesh implant surgery including severe and disabling pelvic pain.
In November 2017, the Therapeutic Goods Administration (TGA) in Australia finally banned 45 pelvic mesh devices including vaginally-implantable prolapse mesh devices and certain mesh slings following the international pelvic mesh fiasco (McCarthy, 2017).
For more information, please watch the 17-minute video by BBC News called ‘NHS sued over vaginal mesh implants’ (18 April 2017).
Several vaginal mesh victims including Kath Sansom (journalist, campaigner and founder of Sling the Mesh) and a urogynaecologist who specialises in mesh excisions are featured in this video.
THREE (3) STUDIES OFFER GOOD NEWS FOR SOME FAILED MESH IMPLANT PATIENTS
Overview
Patients suffering from severe pain and other serious complications due to failed mesh implants may explore whether mesh removal surgery (i.e. mesh excision) is a viable option to remove all or part of the mesh implant.
Click to access ExcisionOfMesh.pdf
https://urogyn.coloradowomenshealth.com/patients/library/transvaginal-mesh-removal
Three (3) mesh removal and/or suburethral tape removal studies, being American, French and Dutch studies, are discussed below:
An American Vaginal Mesh/Suburethral Tape Removal Study
An American study analyzed the results of 123 patients who had surgery to remove vaginal mesh (N=69; the mesh group) or synthetic suburethral tape (N=54; the tape group) in a bid to reduce pain during 2005 to 2013.
The average visual analog score (VAS) score was reduced from 7.9 (before surgery) to 0.9 after removal surgery in the mesh group, as revealed during follow-up 6 to 47 months later.
Meanwhile, the average VAS score decreased from 5.3 (pre-surgery) to 1.5 after removal surgery in the tape group, as revealed during follow-up 6 to 59 months later.
Best of all, 81% of the tape group and 67% of the mesh group were completely pain-free after their respective surgeries!
The authors concluded that if pain is the only reason for surgery to remove either suburethral tape or vaginal mesh, it is likely then that significant pain relief will result following removal surgery (Hou et al, 2014).
A French Mesh Removal Study
A French mesh removal study revealed that mesh can be removed both safely and efficiently in many patients, with operating times averaging only 21 minutes. (NB Some mesh removal operations may require several hours to perform.)
Specifically, 61 of 83 mesh patients underwent complete mesh removal. Fifty-eight (58) mesh excisions were done more than 2 years after the mesh was implanted in the first place (Marcus-Braun and von Theobald, 2010).
A Dutch Mesh Excision Study
A Dutch study analysed 73 mesh-implanted patients who underwent partial or complete mesh excision. Thirty (30) patients had complete mesh removal while 43 patients underwent 51 partial mesh operations.
Prior to their mesh removal surgery, 77% suffered severe pain including vaginal pain, vaginal bleeding/discharge, pain during sex as well as lower abdominal, back, buttock and/or leg pain.
Positive outcomes including symptom relief were achieved for 92% of the 73 patients.
Specifically, 70% of those patients who underwent complete mesh excision and 60% of those who had partial mesh excision enjoyed COMPLETE RELIEF from mesh-related symptoms.
As with all surgeries, there are inherent risks and complications that may be involved with mesh excisions. Furthermore, pelvic organ prolapse or stress urinary incontinence may recur (Tijdink et al, 2011).
Further to Aforementioned 3 Studies
Please note that whilst the results from the American, French and Dutch studies appear very encouraging, it is not known whether these results can be extrapolated and/or whether these results are representative of the norm. More studies are required.*
Each mesh victim who seeks medical advice regarding mesh excision surgery needs to be individually assessed by a highly skilled medical specialist and/or by a mesh removal medical centre (that may or may not be nearby).
Whilst there is always hope, mesh removal surgery may not always be an option due to excessive risks and complications inherent in certain individuals.
However, until one knows for sure, ‘it is usually better to look at the glass as being half full than half empty’.
At the end of the day, botched mesh implants is a collective human issue, and not just an individual problem. As such, we are all in this ‘mesh mess’ together … not just the mesh victims themselves.
Kath Sansom’s Story Including Removal of Vaginal Mesh Implant
Kath Sansom is a journalist and mom of two who used to enjoy high-board diving, boxing and mountain biking.
In March 2015, Kath had a vaginal mesh implant for mild stress urinary incontinence caused by childbirth.
 Kath Sansom, journalist, campaigner and founder of Sling the Mesh
Kath Sansom, journalist, campaigner and founder of Sling the Mesh
Source: https://news.sky.com/story/journalist-kath-sansom-was-wreck-after-vaginal-mesh-implant-11086123
As soon as her mesh sling was implanted, Kath felt pain. In her words,
‘The pain was instant. I struggled to walk. The pain down the backs of my legs felt like really deep, heavy toothache. It hurt me to walk, sit, lie. I couldn’t get any relief. I had cheese-wiring pains in my vagina, burning pain so bad I couldn’t even use a tampon. In the weeks before, I did a boxing class, high-board diving and mountain biking. I went from that to excruciating pain … it gradually got worse and worse.’
Kath felt betrayed because the true risks of vaginal mesh implants were never revealed to her prior to surgery. She said she would have ‘run out the door’ if only someone had said (quoting),
‘You can have this little operation but you might lose your sex life.’
or
‘You can have this little operation and you might not be able to walk – but at least you won’t wee your pants.’
Kath Sansom had her botched mesh sling removed 7 months later. In her words (quoting),
‘I got a lot better, although I’m right up there at the good end of recovery compared with other women. I can still swim. But even so, it’s a new normal. I have to be very careful when putting impact on my legs, I have to be careful how I move. If I overdo things I can end up in pain the next day and having to take strong painkillers. I’ve got all these pain relievers in my bag just in case …’
‘You go from being a healthy mum with a bit of an embarrassing problem, to suddenly your life is turned on its head. And you’ve got to accept that this is now your life because even if you have a mesh removal, you will never go back to the woman you were.’
After her dreadful experience with the now-removed vaginal mesh implant, Kath founded and runs the Sling the Mesh campaign group that has over 7,300 members (Sansom, 2017; Brown, 2018; Sansom, 2018; Briggs, 2019; Sling the Mesh).
Catie’s Story Including Removal of Mesh Implant
The following is a story about Catie in New Zealand who underwent 3 operations in an effort to remove all mesh.
Catie’s pelvic mesh was initially implanted without incident. However, 2 years later, (quoting Catie) ‘[the mesh] was rotting and eroding inside …’, causing pain and discharge. At first, Catie was treated for a potential STD (which wasn’t the case at all) via ‘many courses of metronidazole’, an antibiotic with terrible side effects.
Several years later in March 2011, Catie finally underwent her first mesh removal surgery. The partial mesh excision took 5 hours because (in Catie’s words) ‘[the mesh] was so ‘stuck’ on in bits and the surgeon had a lot of difficulty getting it out’.
By August 2012, Catie had 2 more excision surgeries.
After her third (and hopefully final) excision surgery that involved ‘a good clean out’ and a D&C, (quoting Catie) ‘there [was] no revolting discharge and … no pain’.
In Catie’s view, it may be another year or more before she will have fully recovered. She credits her mesh removal surgeon for being wonderful.
Formerly a triathlete, Catie is struggling to become active again. Nonetheless she is grateful for feeling better after a very long and painful journey.
Catie’s Story:
http://meshdownunder.co.nz/kiwi-stories
Claire Daisley’s Story – Mesh Removal Surgery by Dr Veronikis
Claire Daisley, a 49-year old mother of 3 in Greenock, Scotland, suffered severe pelvic pain following mesh implant for bladder weakness after childbirth 9 years ago in 2010. She used crutches and wheelchairs due to unbearable pain. Climbing stairs was a nightmare. Claire even considered suicide to end all her suffering.
After her mesh implant, Claire became doubly incontinent. Furthermore, she developed osteoarthritis, autoimmune issues and other medical problems.
Following surgery in Scotland to remove only 1/3 of her mesh, Claire was told that it was all gone. Unsurprisingly, her pain and other medical issues persisted.
Claire was then told that both her bowel and bladder had to be removed at the end of July 2019.
Fortunately, Claire received a phone call from Dr Veronikis’ office to fly to the US for complete mesh removal surgery at around the same time. Dr Dionysios Veronikis (aka Dr V) is a Harvard-trained obstetrician-gynecologist who specialises in Female Pelvic Medicine, Reconstructive Surgery, Obstetrics and Gynecology. He is based at the Vaginal Surgery and Urogynecology Institute at Mercy Hospital in St. Louis.
Needless to say, Claire cancelled her bowel and bladder removal surgery in Scotland and instead, flew to the US for complete mesh removal surgery by Dr V.
Dr Veroniki was able to remove all of the remaining mesh (i.e. 13 cm of residual mesh) after a 4-hour operation. Furthermore, her bowel and bladder were saved by Dr V.
Given Claire’s dire circumstances, Dr Veroniki performed the mesh removal surgery for free while generous donors paid for her flights, accommodation and hospital fees.
After waking up from surgery, Claire said,
‘Hi, my surgery is all over. My mesh is gone. 13 cm was removed.
So, back in Scotland [when 1st mesh removal surgery was done], to be told that I had a full mesh removal, that there was none left, is shocking!
Claire continued,
‘I have been, and I’m not home a week yet … there’s a difference in my skin that was almost immediate. So things are starting to happen, from having [all the mesh] removed.
For the first time in 9 years, I actually have hope for the future. And I think it’s something that everybody that’s been mesh-injured deserves.
When you’re in so much pain, you don’t have that hope. It’s just an existence.
Now that this is gone, completely mesh-free, there’s hope for the future.’
Claire added,
‘They have not just changed my life, they have saved my life, and I cannot thank them enough. It is hard to believe that only a few months ago, I was in agony and utter despair. I am transformed.
I’m overjoyed that I did [put my trust in Dr V], and thanks to his skills and the … people who donated money … for me to go to the US, I feel like a new woman.
Dr V must be allowed to help other women like me. I’m the living proof.’
For full story including 4-minute video, see:
- Scott, Marion. Video by Megan McEachern.
Crippled in Scotland, saved in the States … Mesh victim Claire Daisley shares her story in today’s Sunday Post. Sunday Post (8 Sept 2019).
- Scott, Marion. ‘This surgery did not just change my life, it saved my life’. Sunday Post (8 Sept 2019).
- Scott, Marion. World-leading mesh surgeon reveals months of talks have failed to fix his trip to Scotland despite minister’s pledge. Sunday Post (8 Sept 2019).
Disclaimer: The story above is not an endorsement of, nor a recommendation for, Dr Dionysios Veronikis (nor any other doctor or medical specialist, for that matter). This story, nor any other patient story, does not imply medical advice. It is a story, and hence, it should be read as such.
Patients should always see their doctors for their personal medical care.
Estelle’s Story – Another Mesh Removal Surgery by Dr Veronikis
Despite 4 surgeries that only removed part of her polypropylene mesh, Estelle Tasz (38) suffered ongoing pain.
Estelle visited Harvard-trained Dr Dionysios Veronikis for the first time at the Vaginal Surgery and Urogynecology Institute at Mercy Hospital in St. Louis. A few days later on 5 August 2014, Dr Veronikis operated on Estelle to successfully remove all of her remaining polypropylene mesh (i.e. transvaginal mesh). Specifically, Dr V removed 17 cm of residual mesh during the 4.5-hour surgery.
In Estelle’s words,
‘Finally, I was told the truth. Finally, I met a doctor who cares, who is a doctor by all meanings of that definition.’
Estelle continues,
‘I feel empty but I feel full. It’s the weirdest feeling, it’s gone, it’s gone. I have a full life ahead of me and Dr. V gave me hope. He saved my life, as a mom, I can’t thank him enough for that.’
For the full story, see:
Akre, Jane. Estelle Finds Complete TVT Removal. Mesh News Desk (12 August 2014).
https://www.meshmedicaldevicenewsdesk.com/estelle-finds-complete-tvt-removal/
Disclaimer: The story above is not an endorsement of, nor a recommendation for, Dr Dionysios Veronikis (nor any other doctor or medical specialist, for that matter). This story, nor any other patient story, does not imply medical advice. It is a story, and hence, it should be read as such.
Patients should always see their doctors for their personal medical care.
WARNING – DO NOT UNDERGO RISKY MESH IMPLANT SURGERY
Many Patients Including an Australian Woman, Jan Wise, Suffer from Pain and Other Complications Following a Botched Mesh Implant
ALL WOMEN, both young and young-at-heart, should be DISCOURAGED from undergoing surgical mesh implants in the first place. Full stop. End of story.
The high risks and serious complications can be catastrophic, post-mesh implant surgery. Mesh implants can cause permanent, disabling and incapacitating pelvic injuries as well as severe, intractable pelvic pain.
Quoting Jan Wise (who now suffers from back and leg pain thanks to a botched implant surgery involving a pig intestine pelvic mesh device in 2012):
‘[I am] rotting from the inside … shooting electrical shock pain from my lower body up through to my head … hoping the thoughts of the nightmare won’t take up too much of [every] day. I allow myself only one period of sadness and crying per day’ (McCarthy, 2017).
Post-implant, in addition to severe pain, Jan suffers ongoing incontinence, a collapsed vagina, (quoting Jan) ‘putrid seroma discharge’ and ‘pelvic discharge with a foul smell’ as well as loss of intimacy with her husband. In her words, ‘It’s a dreadful mess down there.’
Some women require pain killers and benzodiazepines as well as regular catheterisation (due to a lost ability to urinate following a failed implant). Many suffer chronic incontinence together with ongoing urinary tract and vaginal infections, discharge and granulomas. Others require enemas for chronic bowel problems. Punctures or lacerations of vessels, nerves, bladder, urethra, bowel, organs and other structures may occur. Mesh implants often erode into the vagina rendering sex impossible with their husbands or partners.
In some instances, exposed mesh may even cause pain and injury to the male partner during intercourse (McCarthy, 2017; Stern, 2017 – in German).
Sadly, the list of mesh-related severe complications never seems to end.
A Young Canadian Mom, Chrissy Brajcic, Loses Her Life Due to Mesh Complications
One Canadian mother of two young children has died at only 42 due to complications including heart failure and sepsis following pelvic mesh surgery to treat childbirth-induced incontinence (McCarthy, 2017).

Chrissy Brajcic (deceased at only 42 following mesh implant complications)
Source: https://www.independent.co.uk/news/uk/transvaginal-vaginal-mesh-surgery-stress-urinary-incontinence-sui-uti-tvt-antiobiotic-resistance-a8092006.html
A Canadian Woman, Nonie Wideman, Changes her Mind About Committing Suicide Following Emergency Mesh Removal Surgery
Believing to be too great a burden to their family and friends and after giving up hope altogether, some mesh victims commit suicide to end it all (McCarthy, 2017).
A woman from BC, Canada, Nonie Wideman, had emergency surgery that successfully removed the intact mesh only. Sadly, the countless, small eroded mesh fibre pieces could not be surgically removed.
Despite intact mesh removal surgery, Nonie still suffers from chronic pelvic and low back pain including burning pain and inflammation. This is likely due to the numerous tiny pieces of eroded mesh fibres that still remain within her pelvic area.
The good news is that Nonie is no longer contemplating suicide. Instead, she is now an advocate for women suffering from mesh-related pain, disability and disfigurement.
In Nonie’s words,
‘Women are often not believed about how mesh is causing them pain or how much pain the mesh is causing them … We do … suicide watches when women start talking like they’re done, they’re finished, they can’t go on anymore’ (Akre, 2012; Favaro, 2018; Favaro & St. Philip, 2019; Welk et al, 2019).
Many Men Also Suffer Pain and Other Complications Following Botched Hernia Mesh Surgery
Over a dozen hernia patients, mainly men, in Australia suffer severe pain, agony, depression and other complications following botched hernia mesh implant surgery.
The following men share their failed hernia mesh implant stories:
John Coady
John Coady underwent hernia-repair surgery in the mid-1990’s. While at work in early 2010, John suffered a mesh-related complication for the first time. Sadly, the follow-up mesh surgery was a complete disaster and immediately resulted in constant pain and other problems. Quoting John,
‘Before the surgery I was happy, worked six days a well and was always busy … Now I am on morphine and just sit around in pain … After the surgery, my entire groin area including my penis and scrotum was black and I was in excruciating pain … It was like I’d been punched in the genitals. They were just black and just swollen beyond recognition … As the weeks turned into months, I was still suffering from immense pain and suffering.’
The surgeon was unable to alleviate the mesh-related pain and other medical issues despite John seeing the surgeon at least once a week for more than 6 months.
In John’s words,
‘… after about six months, the surgeon told me that there was nothing wrong with me … [adding] ‘I’ve done my job’ and to go away.‘
Dominic’s ‘Five Years of Hell’ Following Failed Hernia Mesh Surgery
Following a botched hernia-mesh operation in 2013, Dominic (46) was left with (quoting) ‘nothing but problems with my bladder’ including pain, incontinence and urine odour. Consequently, his social life including intimacy was virtually non-existent.
George
George, another hernia mesh victim, stated that 2 years after mesh surgery, ‘the mesh got tangled with [his] bowel. He added:
‘I was vomiting this black stuff and I had a tube down my throat. I was in hospital for a week … surgeon … remove[d] all the mesh that was in my stomach. Since then, hernias kept popping out …’
Phil
Phil suffered ongoing pain in his right leg since undergoing mesh implant surgery to repair hernia years ago.
Successful Mesh-Free Surgery for Bob Wolf, Hernia Patient
While most failed mesh implants affect women, some men also suffer following hernia mesh implants.
A mesh-free hernia surgery that was developed by an American surgeon, Dr Mohan Desarda, is now performed by many clinicians.
One satisfied American patient, Bob Wolf, underwent mesh-free hernia surgery 3 years ago in Las Vegas. He decided to have no-mesh hernia repair after his friends told him about their pain and suffering following hernia mesh implant.
In his words,
‘I am 76, running full speed, every day at work and play’
(Wakatama, 2018).
WHAT OPTIONS EXIST, POST-MESH IMPLANT?
If chronic pelvic pain persists, surgical removal of the implanted mesh may be the only effective treatment option for some patients (see aforementioned American, French and Dutch studies). Unfortunately, it may not always be possible to remove all of the mesh without also damaging nearby organs and tissues. In other words, there may be residual mesh that is simply too risky to remove.
OPTIONS TO CONSIDER OTHER THAN MESH IMPLANT SURGERY
Options to try before even thinking about the unthinkable vaginal mesh implant surgery include:
Non Invasive Options
- Pelvic floor exercises, also known as Kegel exercises (named after Arnold Kegel, a US gynaecologist). Kegel exercise can be taught and supervised by a physiotherapist or continence adviser, and done daily at home (Ward, 2018);
- Yoga and pilates that aim to strengthen the pelvic regions;
- Acupuncture for stress urinary incontinence (e.g. Hui Yin acupoint, CV1, Meeting of Yin) ** *** (Kim et al, 2011; Zhu, 2011);
- Incontinence pads (many women opt for this non-invasive option);
- Substitute action sports (e.g. soccer, tennis) for gentler physical activities that may lead to less ‘leakage’ … and don’t stress if there is residual ‘leakage’. After all, that is what incontinence pads and showers are for;
- Maintain a healthy diet, lose weight, stop smoking and ensure good quality of sleep. This is important for optimum autonomic nervous system function including high vagal output throughout the body including in the pelvic region; and
- If concerned, see your family doctor.
Surgery Without Mesh Implant
- Surgery that does not involve mesh implants, in particular, synthetic mesh implants (Bang & Belal, 2016).
In conclusion, please avoid vaginal mesh implants altogether. The risk is too high that severe pelvic pain and other serious injuries may result, post-mesh implant (Heymann et al, 2019).
IS SURGERY TO REMOVE BOTCHED MESH IMPLANTS A VIABLE OPTION FOR SOME PATIENTS?
Like all surgeries, removal of failed mesh implants has inherent risks. As such, some mesh victims may prefer not to consider excision surgery.
Mesh removal surgery may not be in the best interest of mesh victims where the risk of injury is high.
Having said that, mesh victims are encouraged to seek medical advice from urogynaecologists and other medical professionals who specialise in mesh excisions.
A Urogynaecologist in the UK Talks About Vaginal Mesh
A urogynaecologist in the UK named Dr Sohier (Suzy) Elneil, has performed over 250 tension-free vaginal tape (TVT) removal surgeries since 2004. This plastic implant is often used for incontinence.
When Dr Elneil met her first mesh patient with severe pelvic pain in 2004, the mesh implant (TVT) had already disintegrated. Following complex surgery to remove the degraded mesh, the patient was finally pain free and able to return to a normal life.
Dr Elneil described another patient, a lawyer who suffered severe pain since undergoing a mesh implant 6 weeks earlier. By the time Dr Elneil saw her, the lawyer was no longer able to work. Alarmingly, she was also suicidal.
Quoting Dr Elneil,
‘As I was operating on her, I could see the tape was embedded into the tissues and there was ulceration in places — doing the surgery was not nice. I kept thinking: ‘How did it get this bad in six weeks?’. Cases like this keep me going — why in this day and age women should be suffering so makes me very angry.’
Dr Elneil describes mesh removal surgery as,
‘…really hard surgery because the mesh gets embedded in the muscles and everywhere. Even though we scan our patients, you never know what you will find until you open the lady up — and sometimes it can be quite upsetting. To be honest, on occasions I feel bereft because I feel so emotional about it; you realise how much this woman must have been suffering.’
In reply to the journalist’s question about when she’d last had a proper holiday, Dr Elneil replied,
‘But if I go on a long break, it means more women might be left waiting in pain, and I can’t have that’ (Brown, 2018; Elkins, 2018).
There are a number of compassionate urogynaecologists, mesh removal surgeons and other medical professionals who specialise in mesh excision. Please see your doctor if you need a referral.
Disclaimer: The story above is not an endorsement of, or a recommendation for, Dr Sohier (Suzy) Elneil (nor any other doctor or medical specialist, for that matter). It is merely a story, and hence, it should be read as such only. (References are provided.) Patients should see their doctors for referrals to specialists, if they wish to do so.
SUMMARY
Australian Senator, Derryn Hinch, once stated ‘Transvaginal mesh is one of Australia’s greatest medical scandals’ (Marwick, 2017).
Others call it ‘the new thalidomide’.
Still others say, ‘Transvaginal mesh is the biggest scandal affecting women since thalidomide’.
Dr Dionysios Veronikis, obstetrician-gynaecologist (mentioned earlier), stated,
‘…mesh is the single darkest chapter in gynaecological surgery and I will do all I can to help free as many women as possible from pain (Scott, 2019).
Dr Veronikis continues,
‘Mesh prolapse kits were just a bad idea. I don’t kow why so many went down that road. With all those mesh arms and a massive amount of mesh and the one size fits all approach. Every woman is different … [mesh prolapse kits] are defectively designed’ (Akre, 2014).
When asked why he never implanted a vaginal mesh device, Dr Frank Gamberdella (1943 – 2019), gynaecologist, Santa Barbara (50 years of clinical experience), replied,
‘I felt it in my hands, and it wasn’t a device that belonged near the vagina.’ Wise man!
Dr Gamberdella belonged to a generation of physicians who were trained to offer autologous slings (i.e. sourced from self) for the treatment of stress urinary incontinence and non-mesh surgery for pelvic organ prolapse. Mesh should be banned altogether and consideration should be made to return to Dr Gamberdella’s non-mesh surgeries (Survivors with Catastrophic Pain, 2019; Isbert et al, 2003; Bang & Belal, 2016; Baylón et al, 2017; Heymann et al, 2019).
Legal class action suits exist all around the world including lawsuits involving more than 100,000 women in the US alone. Legal bills are expected to exceed $20 billion. This clearly demonstrates the unacceptably high risks of mesh implants.
Vaginal mesh is no longer used in Australia, Ireland and Scotland (Berger, 2019).
To protect all women, mesh implant operations should be banned altogether (McCarthy, 2017). The risks of mesh surgery including disabling pelvic pain, compromised or non-existent sex life, loss of enjoyment of life, suicide and death certainly outweigh any purported benefits.
Finally, women who are adversely affected by pelvic pain due to mesh implants may consider whether mesh excision is an option. In other words, if chronic pelvic pain persists, surgical removal of the implanted mesh may be the only effective treatment option for some patients (see aforementioned American, French and Dutch studies).
It may not be possible to remove all of the mesh without also damaging nearby organs and tissues in some women. There may be residual mesh that is simply too risky to remove. Thus, mesh removal may not be an option for some patients.
I hope that this blog post (that also mentions 3 mesh removal studies, being American, French and Dutch, may offer light at the end of a very long dark tunnel for some women.
Remember that you are NOT alone! As a global community, we are ALL in this together! If you are a mesh implant victim, please reach out for support.
Please help spread the word that this mesh mess is no longer acceptable. Specifically, synthetic mesh implants should be banned altogether.
Sabina Walker
Blogger, Pain Matters (in WordPress)
PS If you believe that this information may help someone, please share this blog post via Twitter, LinkedIn, Facebook, etc.
And please tell this person to never, ever give up!
KEY
* If I find additional mesh removal studies, I will add another blog post to highlight these studies. If you are interested in my updates, just ‘Follow’ this blog and/or my Twitter.
** Acupuncture Helps Bladder Control, Stops Leakage. HealthCMi (12 October 2016).
*** Reiki Master Attunement Exercise
https://www.liannegraham.com/wp-content/uploads/2017/03/Hui-Yin-Exercise.pdf
REFERENCES
Hope for Mesh Patients
Medical Papers and Articles – Corrective Surgery to (Partly or Fully) Reverse Failed Vaginal Mesh Implants
An American Mesh Removal Study
(1) Hou et al. Outcome of transvaginal mesh and tape removed for pain only. J Urol (Sept 2014); 192(3): 856-60.
doi: 10.1016/j.juro.2014.04.006.
https://www.ncbi.nlm.nih.gov/pubmed/24735934
A French Mesh Removal Study
(2) Marcus-Braun, N and von Theobald, P. Mesh removal following transvaginal mesh placement: a case series of 104 operations. Int Urogynecol J. (April 2010); 21(4): 423-30.
doi:10.1007/s00192-009-1050-3.
https://www.ncbi.nlm.nih.gov/pubmed/19936589
A Dutch Mesh Excision Study
(3) Tijdink et al. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Int Urogynecol J. (Nov 2011); 22(11): 1395-404.
doi:10.1007/s00192-011-1476-2.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3187855/
Other Papers
(4A) Bang SL, Belal M. AUTOLOGOUS pubovaginal SLINGS: back to the future or a lost art?. Res Rep Urol. 2016;8:11–20. (2016 Jan 18). doi:10.2147/RRU.S96957
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723033/
(4B) Isbert et al. Die Implantation von Polypropylene-Mesh induziert eine B7-2 (CD86) positive Fasciitis am Rattenmodell. [Polypropylene mesh repair for treatment of groin hernias induces a B7-2 (CD86)-positive fasciitis in rats.]
In: Menger M.D., Haas N.P., Neugebauer E., Bauer H. (eds) Chirurgisches Forum 2003 für experimentelle und klinische Forschung. Deutsche Gesellschaft für Chirurgie, vol 32. Springer, Berlin, Heidelberg.
https://link.springer.com/chapter/10.1007/978-3-642-19024-7_141#citeas
(4C) Baylón et al. Past, Present and Future of Surgical Meshes: A Review. Membranes (Basel) (22 Aug 2017);7(3):47.
doi:10.3390/membranes7030047
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618132/
(4D) Heymann et al. Polypropylene mesh implantation for hernia repair causes myeloid cell-driven persistent inflammation. JCI Insight (24 Jan 2019); 4(2): e123862. doi:10.1172/jci.insight.123862
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6413778/
(5A) Stetson, Diana. Vaginal Mesh Excision. Department of Obstetrics and Gynecology, von Voigtlander Women’s Hospital, Michigan Medicine (May 2018).
Click to access ExcisionOfMesh.pdf
(5B) Transvaginal Mesh Removal. Colorado Women’s Health, University of Colorado Hospital.
https://urogyn.coloradowomenshealth.com/patients/library/transvaginal-mesh-removal
A UK-Based Patient, Kath Sansom, Has Mesh Removal Surgery
(6A) Brown, Julia. ‘The pain was instant’: The devastating impact of vaginal mesh surgery. NewScientist (5 Sept 2018).
(6B) Sansom, Kath. Journalist Kath Sansom was ‘wreck’ after vaginal mesh implant. Sky News (30 Jan 2018).
https://news.sky.com/story/journalist-kath-sansom-was-wreck-after-vaginal-mesh-implant-11086123
(6C) Sansom, Kath. Vaginal mesh left me in agony. When will women’s health be taken seriously? The Guardian (27 April 2017).
(6D) Briggs, Caroline. Life after vaginal mesh surgery. BBC (5 April 2019).
https://www.bbc.com/news/in-pictures-47777782
A NZ-Based Patient Undergoes Several Excision Surgeries to Remove All Mesh
(7) Catie’s Story:
Real Kiwis, Real Stories. New Zealand – Mesh Down Under
http://meshdownunder.co.nz/kiwi-stories
Media – Failed Vaginal Mesh Implant Stories
Alison Blake (Suicided Following Botched Mesh Implant)
(1) McCarthy, Joanne.’There was a look in her eyes’: Mother’s emotional torment at surgery nightmare. Sydney Morning Herald (20 December 2017).
Chrissy Brajcic (Deceased At Only 42 Following Failed Mesh Implant)
(2A) McCarthy, Joanne. Canadian woman Christina Lynn Brajcic dies after receiving pelvic mesh implant. Sydney Morning Herald (4 December 2017).
Please watch 2-minute video of Chrissy’s sad surgical mesh story (now deceased at only 42 following mesh-related complications).
(2B) Marsden, Harriet. Vaginal mesh campaigner ‘dies of sepsis after antibiotic-resistant infection’. Independent (4 December 2017).
Jan Wise, A Mesh Implant Pain Sufferer
(3A) McCarthy, Joanne. Pelvic mesh victim speaks out about ‘one of the greatest medical scandals in Australian history’. The Herald (23 March 2017).
http://www.theherald.com.au/story/4547363/its-so-awful-and-so-private-photos-video/?cs=5507
Please watch 3-minute video of Jan’s tragic surgical mesh story.
(3B) McCarthy, Joanne. Pelvic mesh victim speaks out about ‘one of the greatest medical scandals in Australian history’. The Herald (23 March 2017).
https://www.theherald.com.au/story/4547363/its-so-awful-and-so-private-photos-video/
‘The Angel’ in the UK Named Dr Sohier (Suzy) Elneil, Urogynaecologist
(4A) Brown, Julia. The inside story of the vaginal mesh scandal, from top removal surgeon. NewScientist(5 Sept 2018).
(4B) Elkins, Lucy. NHS Health Heroes campaign: Surgeon who works day and night to help women told they imagined their pain. Daily Mail Australia (10 July 2018).
https://www.dailymail.co.uk/health/article-5935393/Surgeon-works-day-night-help-women-told-imagined-pain.html
Other Articles and Stories from Media
(5A) Marsden, Harriet. The biggest NHS scandal you’ve never heard of only affects women, but men should be just as concerned. Independent (5 August 2017).
(5B) Marsden, Harriet. Panorama investigation reveals medical company failed to fully inform doctors of vaginal mesh risks. Independent (11 December 2017).
(6) Moss, Rachel. What is A vaginal mesh implant? Government to launch audit into complications. Huffington Post (30/1/2018).
(7) McCarthy, Joanne. Pelvic mesh left a man ‘stabbed’ during sex, regulator warned. The Herald (17 March 2017).
http://www.theherald.com.au/story/4535453/mesh-in-stabbing-incident/?cs=5507
(8) McCarthy, Joanne. Australian pelvic mesh victims launch their case against Johnson & Johnson. The Herald (4 July 2017).
http://www.theherald.com.au/story/4769450/pelvic-mesh-victims-in-landmark-action/?cs=2452
(9) Moodie, Claire. Vaginal mesh implants: Gynaecologist urges proactive response to health concerns. ABC News (4 July 2017).
http://www.abc.net.au/news/2017-07-04/vaginal-mesh-implants-surgeon-urges-proactive-response/8677488
(10) McCarthy, Joanne. Johnson & Johnson pelvic mesh doctor said he would not want his wife to undergo procedure, Federal Court told. Sydney Morning Herald (5 July 2017).
(11) Pelvic implant lawsuit underway in Sydney. 9 News (4 July 2017).
http://www.9news.com.au/national/2017/07/04/08/57/vaginal-mesh-lawsuit-to-commence
(12) Smith, Leesa. ‘Vaginal mesh implant has destroyed my life — it’s just so hard to go on’. News (11 May 2017).
(13) For Donna’s, Catie’s, Helen’s and other mesh victim’s stories, please see:
Real Kiwis, Real Stories. New Zealand – Mesh Down Under
http://meshdownunder.co.nz/kiwi-stories
Please note: Catie’s story involving complete mesh removal may offer hope to other mesh patients.
(14A) Favaro, Avis. Woman appeals to Ottawa for temporary ban on female pelvic mesh. CTV News (8 January 2018).
(14B) Favaro, Avis & St. Philip, Elizabeth. Women with pelvic mesh complications at higher risk of depression, suicidal thoughts. CTV News (9 January 2019).
(14C) Akre, Jane. Wideman – Canadian Child Advocate and Rancher. Mesh News Desk (21/5/2012).
(14D) Welk et al. Association of Transvaginal Mesh Complications With the Risk of New-Onset Depression or Self-harm in Women With a Midurethral Sling. JAMA Surg (9 January 2019).
doi:10.1001/jamasurg.2018.4644
https://jamanetwork.com/journals/jamasurgery/article-abstract/2719817
(15) Wakatama, Giselle. Concern grows over hernia mesh as more patients share post-surgery horror stories. ABC News (14 Sep 2018).
(16) Marwick, Jane. Why aren’t we talking more about one of Australia’s greatest medical scandals? The Daily Telegraph (29 August 2017).
(17) Hooton, Amanda, & McCarthy, Joanne. The ‘eight-minute’ cure: how transvaginal mesh sentenced thousands of women to a life of pain. SMH (15 June 2019).
(18) Hennessy, Michelle. Vaginal mesh implants: Women complain of delay in aftercare for severe complications. The Journal (16/6/19).
https://www.thejournal.ie/vaginal-mesh-aftercare-4682615-Jun2019/?utm_source=shortlink
(19) Scott, Marion. Acclaimed surgeon offers to come to Scotland to ease agony of mesh victims. Sunday Post (14/1/2019).
(20) Akre, Jane. Estelle Finds Complete TVT Removal. Meshnewsdesk (12/8/2014).
https://www.meshmedicaldevicenewsdesk.com/estelle-finds-complete-tvt-removal/
(21) Left Behind by the Vaginal Mesh MDL: Survivors with Catastrophic Pain (14 July 2019).
Pelvic Mesh Support Groups
(1) Sling the Mesh – Raising awareness of the life changing risks of a “simple” day case operation
https://slingthemesh.wordpress.com/media-news-updates/
(2) Australia – Mesh Down Under
https://www.facebook.com/MeshDownUnder/
(3) New Zealand – Mesh Down Under
(4) Patient Groups: Pelvic Mesh. The Independent Medicines and Medical Devices Safety Review (Dec 2018); Pages 1 – 317.
Click to access FOR%20PUBLICATION%20Patient%20Groups%20-%20Pelvic%20Mesh.pdf
Kegel Exercises For Weak Pelvic Floor Muscles
(1) Ward, Mary. A weak pelvic floor can mean more than a little leakage. Sydney Morning Herald (18 June 2018).
Acupuncture for Stress Urinary Incontinence
(1) Kim et al. The Effect of Needle-embedding Therapy and Pharmacopuncture Therapy on Patients with Urinary Incontinence. Journal of Acupuncture and Meridian Studies (Dec 2011); 4(4): 220-4.
https://doi.org/10.1016/j.jams.2011.10.012
https://www.sciencedirect.com/science/article/pii/S2005290111000458
(2) Zhu, Angela Tian. The Million-Dollar Point. Traditional QI Energy (13 May 2011).
https://www.traditionalqi.com/2011/05/13/the-million-dollar-point-2/
In German
(1) Wenn die Vagina plötzlich zubeißt [translated: When The Vagina Suddenly Bites]. Stern (21 March 2017).
Thanks To Dr Katinka’s Non-Invasive Treatments, Many CRPS Patients Are Enjoying Significant Recovery From CRPS
Feature Image of Dr Katinka van der Merwe sourced from:
Dear Pain Matters blog readers,
As mentioned in earlier posts, Dr Katinka van der Merwe (aka Dr Katinka), a Chiropractor at The Neurologic Relief Center (aka Spero Clinic), Arkansas, USA, specializes in chronic pain including complex regional pain syndrome (CRPS). Dr Katinka’s novel and non-invasive approach focuses on restoring balance in the autonomic nervous system, with particular emphasis on the vagus nerve (‘the wandering nerve’). As a result, Dr Katinka’s treatments may successfully reduce, and even eliminate, pain and inflammation as well as enhance function and mobility in many CRPS and other pain patients. In doing so, she has literally given back their lives!
Dr Katinka’s unique medical talents for treating chronic pain are amongst the best in the world. Furthermore, Dr Katinka’s compassion and empathy for each of her patients adds a touch of humanity to a field of medicine that (all-too-often) appears disengaged and disconnected with the actual depth of pain and suffering endured by so many chronic pain patients.
This blog post will review 10 CRPS patients who were successfully treated by Dr Katinka. I urge the reader to watch at least some of the YouTube links. Like me, you will (likely) be very touched by their stories of recovery from CRPS.
It is exciting to reveal that 7 of these 10 patients achieved COMPLETE pain relief following Dr Katinka’s 10-week treatment program! Please click on the following table to view a summary of 7 CRPS patients who now enjoy nil pain.
Table – 7 CRPS Patients Who Recovered From CRPS
The following 3 CRPS patients enjoyed significantly less pain following completion of Dr Katinka’s 10-week treatment program:
- Debbie (retired), whose pain levels no longer exceed 2;
- Kristin, whose pain levels were 2, post-treatment, compared to 7, pre-treatment; and
- Billi, who was finally able to extend her left leg, post-treatment.
Details of 10 CRPS Patients Successfully Treated By Dr Katinka
1. Carlos’ CRPS Story
Carlos was in a serious auto accident in 2005 that resulted in spinal cord injury and other injuries as well as constant and severe pain for 7 years. He was formally diagnosed with CRPS 2 years later in 2007. His CRPS started in his abdominal area and affected his entire digestive system. His CRPS spread throughout his entire body following TENS treatment.
Carlos had to use a wheelchair and a cane due to severe pain from CRPS. He was unable to eat solid food. Drinking water even hurt. His eyes had a constant burning sensation and he became sensitive to light. Having said that, he was grateful that his vision remained unaltered.
Carlos tried everything to control his pain including pain medications, spinal injections, epidurals and a spinal stimulator implant. Unfortunately, his severe pain levels exceeding 10 continued to torture him.
Despite Carlos having given up on hope and even on life itself, his wife convinced him to see Dr Katinka as a last resort. When Dr Katinka met Carlos for the first time, he was unable to eat more than a couple spoons of chicken broth at a time. The latter even caused hours of excruciating pain for Carlos.
Quoting Dr Katinka,
‘Carlos was white as a sheet, and utterly without hope. His pain was carved into his face for the world to see. He came in with his wife. She told me that she was afraid that Carlos would take his own life if they could not find relief soon. She had convinced him to try just one more doctor. With them that day was their nine-month old baby, Sean. I remember looking at that little boy and trying to imagine his life without his father in it to see him grow up. Carlos finally looked up and said: ‘You can’t help me. No one can help me. I am here because my wife asked me to come.’ ’
Despite his dire state of health, Dr Katinka proceeded with her gentle upper cervical treatment on him. To both of their surprise and for the first time in 6 years, his pain levels dropped dramatically from a 10 to a 3 following her manual procedure of his upper neck area! Carlos finally obtained relief from his constant burning pain within the first 15 minutes of his first treatment! What a pleasant surprise after suffering severe and constant pain due to full-body CRPS for 6 entire years! To top this off, Carlos celebrated this milestone by finally eating a full-course dinner without pain for the first time in 5 years.
He was a changed man when he came back for his second day of treatment. His colour had returned as did his ‘life spark’.
After his 3rd day during Week 1 and after only 3 treatment sessions with Dr Katinka, his pain levels dropped to a 2 … and then to a 1. In fact, some parts of his body were not even sensing pain anymore!
After Week 6 at the Center, he was down to only one pain medication (from several pain medications). Furthermore, his pain levels remained at 1 or 2.
Twelve weeks later, Carlos was completely pain-free.
Three (3) years later, Carlos stated that he was still 99% better, and that he no longer needed any pain medications. This demonstrates the lasting benefits of Dr Katinka’s 10-week pain program.
Almost five years later in 2016, Carlos is still pain-free. He is now working as a pastor and travels all over the world. Whilst he has faced physical challenges since then including gallbladder surgery, he has no sign of CRPS returning.
(Carlos was interviewed 3 times by Dr Katinka – twice during his 10-week pain treatment program and a third time 3 years after his successful treatment for CRPS.)
https://www.youtube.com/watch?v=pYE0aW1cTh8
http://seeingyouwell.com/testimonials/
http://rsds.org/new-approach-rsd-crps/
2. Brock’s CRPS Story
Brock suffered CRPS for 10 months following a broken ankle in January 2015. Brock was bedridden for 10 weeks due to excess pain from CRPS that also spread to his other leg. Brock was on crutches for 7 months. By now, his CRPS-affected leg comprised mainly of skin and bone, with only a little bit of calf and thigh remaining. The bulk of his muscle mass in his CRPS-affected leg was gone. Somewhere along the way, Brock also lost his job. Needless to say, CRPS significantly changed his life for the worse in every conceivable way.
In addition to ‘tonnes of medication’, he had 4 sympathetic nerve blocks. Unfortunately, this did not offer the pain relief that Brock needed in order to function properly.
When asked about any neck injuries by Dr Katinka, Brock confirmed that, in fact, he did have a prior neck injury prior to developing CRPS.
Brock described his first treatment during his trial week with Dr Katinka that involved gentle hands-on upper cervical manipulation as follows (quoting):
‘…completely painless, … I’ve had no side effects … no pains from the treatments … Nothing … Amazing.’
Dr Katinka asked him, ‘So your pain level right now is?’
Brock answered, ‘I’m a zero … zero.’ (He laughs.)
Dr Katinka enquired, ‘How does it feel?’
Brock happily replied ‘I’m smiling for the first time in a long time. I haven’t been at a zero in almost a year now … and I’ve been amazed … 5 seconds into the first treatment … I was pain-free.’
Dr Katinka stated, ‘I’m so excited!’
Brock chuckled, ‘Me too … me too!’
https://www.youtube.com/watch?v=MU7ggYcdJO4
3. David’s CRPS Story
David suffered CRPS in his right foot for almost 3 years following right foot surgery to remove a bunion and straighten out a ‘hammer toe’. This was followed by a second surgery to remove a nerve from his right foot due to pain. After these surgeries, David started having severe pain and swelling in his CRPS-affected right foot.
Post-CRPS, David walked with a cane, crutches and/or used a wheelchair due to pain. He has his own wheelchair ramp built behind his house. David was no longer able to drive or do anything else. David was afraid to move for fear of making the pain worse than it already was.
As a result of the severe and unrelenting pain, David became extremely depressed. Quoting David,
‘Depression … got so bad that, twice, I took very seriously about taking my own life … but … [my wife] … told me that there is only one that can give live and one has the authority to take life…’
Whilst his CRPS did not spread, his severe pain levels ranged from 11 to 13 (out of 10).
Quoting David, ‘The pain medications just numb the pain. You have to keep it up, you’re drugged out … can’t do anything … your life is gone.’
In addition to morphine, Oxycontin and Hydromorphone, David also tried nerve blocks, without success.
On his first day at the Center, Dr Katinka asked David to lie on the treatment table for a diagnostic test. As she chatted to David, Dr Katinka applied pressure to his neck and underneath his skull. As she continued to apply gentle pressure in this area, his pain levels started to decrease dramatically until they reached a 2! The pain levels did not, however, stop there. Instead, they dropped even further as Dr Katinka continued to apply gentle pressure. Guess what happened next?? David’s pain levels were finally at zero! Imagine that!! Zilch pain!! Wow!!
After completing his trial (first) week at The Neurologic Relief Center, his right foot no longer appeared red and swollen.
Five (5) weeks later at the Center, David finally enjoyed complete pain relief and his right foot was not swollen. David’s story of recovery from CRPS in his right foot is nothing short of amazing!
During his last 2 days at the Center, David intentionally left his walking cane in his motel room. He was now able to walk on his own 2 feet without pain.
David’s wife, Debbie, said to Dr Katinka, ‘You have … a special heart for people in chronic pain, and it shows.’
Dr Katinka answered softly, ‘Thank you. I do. Especially RSD…’
Before seeing Dr Katinka, David was in so much pain and pain-induced stress. Now that his pain, and the stress relating thereto, was gone, David is finally looking forward to going fishing again on his own fishing boat.
David finally has his life back! What could be better than that??
https://www.youtube.com/watch?v=hWIaMBhcvA0&sns=em
4. Madi’s CRPS Story
Madi, a teenager from Arkansas, sustained serious injuries including a fractured arm in a roll-over car accident 6 years ago when she was only 13. Thereafter, Madi developed CRPS in her fractured arm that spread to her middle to lower part of her back as well as her entire left leg. Her pain was sometimes so severe that she had difficulty walking.
Madi tried many different pain treatments including nerve blocks and lumbar blocks. She has 2 stimulators surgically implanted in her back as well as a pump. Sadly, the 2 stimulators did not reduce her pain levels at all. While the pump offered some relief from her pain, it did not offer the amount of pain relief that she had hoped for or that she needed in order to function properly.
Madi underwent a chemical ablation (ie Phenol neurolysis) to burn her sympathethic nerve. Sadly, this medical procedure only made her pain worse. Madi took medication to help her sleep through the night despite the pain.
Madi felt guilty for being in pain all the time. She felt like a burden to her family.
Understandably, Madi was sceptical about seeing Dr Katinka for the first time. After all, no one else had been able to help her since her serious car accident 6 years ago.
However, Madi’s doubts quickly vanished after her first appointment. When Dr Katinka performed a diagnostic test involving a gentle and non-invasive upper neck manipulation, Madi’s pain levels dropped to zero for the first time in 6 years since her car accident! Wow!! This 100% pain relief lasted for an entire 40 minutes.
Needless to say, after her first day at the Center, Madi was eager to return for more treatments! Even after 2 weeks (including during her YouTube interview), Madi stated that her pain levels were nil! This is great news!
In closing, Madi’s mom said (quoting),
‘There is no amount of money that could ever give us what we have now, and it’s [Dr Katinka] that gave us that … And we talked about how her pain was locked, and how [Dr Katinka had] the key that unlocked it and made it go away…’
(Madi had just completed 2 weeks of her 10-week pain program at the Center when this interview was done.)
https://www.youtube.com/watch?v=IVqSGHwmf-E
5. Scott’s CRPS Story
Scott suffered from CRPS for 2 years following carpal tunnel surgery to his right hand. Scott’s pain extended from his fingertips in his right hand up his right arm and to his neck. His pain levels in his right hand were excruciating and would always reach 8 to 10 by afternoon. Consequently, by the end of each day, he did not want to do anything at all.
Scott’s daily pain medications included massive amounts of Gabapentin and Ibuprofen. He also tried numerous nerve blocks as well as 5 ketamine infusions. While the effects of the first ketamine infusions seemed promising, the actual pain relief offered by the remaining 4 ketamine infusions lasted only 2-3 weeks each.
After only 4 days of treatment with Dr Katinka, the pain from Scott’s right wrist to his neck vanished. While there was some lingering pain in his fingers in his right hand (with pain levels at 1), this was significantly more tolerable than before.
During her gentle hands-on upper cervical manipulation, Dr Katinka confirmed that the right side of Scott’s neck had felt a bit abnormal. Dr Katinka’s chiropractic treatment of Scott’s upper cervical area aimed to ease the pressure on his vagus nerve. In so doing, she increased the activity of his vagus nerve.
Research by Dr Kevin Tracey shows that increased efferent vagal activity can lead to drastically reduced localised inflammation (Walker & Drummond, 2011). This would, of course, include any inflammation in David’s CRPS-affected right hand including fingers. Decreased inflammation often leads to less pain, and in some cases, nil pain.
And this is exactly what happened to Scott during the upper cervical procedure!
In response to her question, ‘What is your pain like?’, Scott replied,
‘Right now it’s a zero.’
Dr Katinka said, ‘Zero! That’s awesome!‘
When Scott was asked whether he had ever experienced nil pain in the past 2 years, he replied that until now, the only time he could not feel his pain was during sleep.
https://www.youtube.com/watch?v=3p1dOOHDuio
6. Barbara Wall’s CRPS Story
Barbara Wall worked as a registered nurse for 25 years. In 2005, Barbara suffered a broken neck due to a severe injury to her cervical spine as well as other injuries. She was also diagnosed with full-body CRPS. Thereafter, Barbara was forced to quit nursing in order to focus on her health issues and constant pain resulting from CRPS, her broken neck and other injuries.
Barbara underwent daily physical, occupational and pool therapy. In addition, she was offered various pain medications, numerous stellate ganglion blocks, lumbar sympathetic blocks and cervical epidural steroid injections, without any success.
Following a successful spinal cord stimulator (SCS) trial, Barbara received an SCS implant. This finally offered some pain relief enabling Barbara to continue with daily physiotherapy plus 2 hours of pool therapy.
Barbara describes 10 years of full-body CRPS as ‘mind blowing, traumatic, overwhelming, and most of all changing’.
Then one day in June 2015, Barbara’s CRPS worsened when she ‘made a simple movement with [her] neck and felt a horrible pop with lightning pain … the pain was intense’. Barbara’s SCS was no longer able to provide pain relief leading to weeks of sleepless nights. Tests finally revealed that 2 of her discs in her neck were so badly damaged that her SCS paddle had shifted to the right, rendering it completely ineffective on the left side. Corrective surgery was considered too risky as it could make her CRPS even worse.
Barbara’s pain levels were at 8 out of 10 when she met Dr Katinka for the first time on 12 October 2015. These pain levels dropped to 4 after her first non-invasive, drug-free and painless treatment with Dr Katinka.
Following completion of Dr Katinka’s 10-week pain program, Barbara’s pain levels are now zero most of the time. Barbara was also able to stop all of her pain medications.
Quoting Barbara:
‘…there is hope in hopeless situations. Even with my continued spine issues and the need for surgery on my cervical spine, I have been able to maintain low to no pain with my RSD. I cannot tell you how amazing it is after ten years of chronic pain to actually sleep throughout the night, to not feel like you are burning from within…’
http://rsds.org/journey-back-health-rsd/
7. Brenda’s CRPS Story
Brenda suffered from CRPS since January 2010 and her pain levels used to range between 8 to 10 ‘pretty much all the time’.
After 4 weeks of non-invasive treatment at the Center, Brenda no longer takes any pain medication. Best of all, Brenda no longer has pain.
(No other details were provided during this short 1-minute YouTube interview.)
http://seeingyouwell.com/testimonials/
8. Debbie’s CRPS Story
Debbie suffered from CRPS for 12 years following a surgical procedure in March 2004. The anesthesiologist had hit a nerve while numbing her frozen shoulder. As a result of severe pain due to CRPS, Debbie was no longer able to work. She also became hypersensitive to clothing including sleeves.
Debbie took many different pain medications including Lyrica and Gabapentin. She also underwent a spinal cord stimulator operation for her pain.
Debbie received frequency specific microcurrent and other non-invasive treatments at the Center from the end of February to May 2016.
Post-treatment at the Center, Debbie feels as if she ‘has a new lease on life … a second chance’. Debbie and her husband were finally able to go on a 3-week road trip that included many rigorous activities such as 5-mile walks.
Debbie’s pain levels are now minimal and no longer exceed 2. Debbie added that she no longer needs Lyrica, Gabapentin nor any other pain medication. She has not turned on her spinal cord stimulator since February 2016.
In Debbie’s words, ‘It’s just amazing!’
(This interview occurred 6 months after Debbie’s successful treatment for CRPS at the Center in 2016.)
https://www.youtube.com/watch?v=yxgG6RfcrRY
9. Kristin’s CRPS Story
Kristin from Pennsylvania suffered from full-body CRPS for 9 years after injuring her T-spine at work.
Kristin tried many different treatments including a spinal cord stimulator trial. However, the spinal cord stimulator had to be removed urgently due to the pain that it caused. Sadly, during its removal, ‘they really yanked on it’. This may have injured the lining of her spinal cord, making her pain worse.
After that, Kristin had numbness and tingling in both hands and arms, both feet and legs as well as on the left side of her face. There was also increased burning pain and she bruised more easily. She couldn’t work anymore due to CRPS. Kristin could only sit and watch TV as well as sleep in the same recliner for years. Sleeping in her bed was no longer a comfortable option.
After treatment by Kr Katinka, Kristen stated, ‘It’s basically been like a miracle. It really has. … The first day, you were able to get rid of pain that I had in my mid back for 9 years.’
Overcome by emotion, Kristin started crying. She continued, ‘I have so much less pain now … my RSD symptoms are still there … but cutting down on medication … I came in at a 7 and today I am leaving at a 2.’
She added, ‘It was definitely worth the 1,200 mile trip that we need, and the money, to come and see you … [Dr Katinka] is the best!’
(Kristin was interviewed on her last day at the Center after completion of Dr Katinka’s 10-week pain program.)
https://www.youtube.com/watch?v=ltc8fUKhmZM
10. Billi’s CRPS Story
Billi is a mother and a flight attendant who can no longer work due to pain from CRPS. Her CRPS affected her entire left arm including hand, wrist, arm and left shoulder for the past 4 years. Billi’s pain levels averaged 3 to 4. Different factors affected her pain levels including daily temperature and activities. Sometimes Billi woke up without pain. However, as soon as she got up and moved around, her pain levels spiked.
Billi tried many pain treatments including bioenergy healing, biofeedback, acupuncture and lumbar injections.
One day, Billi accidentally fell backwards while going down some stairs in Paris, France. This resulted in a hyperstretched nerve in her left leg that prevented her from extending out her left leg while walking.
Amongst different treatments offered at the Center, Billi had frequency specific microcurrent on her left leg. After this treatment, Billi was finally able to stretch and extend out her left leg while sitting and walking.
When asked what CRPS took away from her, Billi replied that CRPS took away her entire life including her beloved job as a flight attendant. She added that she would love to go back to her job. CRPS had also drastically changed her role as a mom.
Dr Katinka added, ‘Our goal is so much bigger than getting you out of pain. It’s getting you back to your life.’
Billi started to weep softly upon hearing these kind and compassionate words. Touched by Billi’s tears of hope and gratitude, it didn’t take long for tears to also start welling up in Dr Katinka’s eyes.
(This interview was done at the end of Billi’s first week at the Center, with more treatments planned and further progress expected for Billi.)
https://www.youtube.com/watch?v=TpMSqe_aXk0
Summary
Dr Katinka strongly emphasizes that The Neurologic Relief Center (aka Spero Clinic) does not aim to:
- Numb the pain;
- Use calmare;
- Use ketamine; or
- Claim to cure CRPS.
Instead, the Center aims to re-balance the central nervous system (CNS), and in particular, the autonomic nervous system including the parasympathetic nervous system (i.e. the vagus nerve). This will allow for optimal healing from within the body. Once the autonomic nervous system balance is restored and vagal outflow increases, reduced inflammation, significant and/or complete pain relief as well as improved function and mobility may arise.
Dr Katinka’s non-invasive treatments for neuropathic pain and injury to the spinal cord include an upper cervical procedure to stimulate the vagus nerve – see below – and frequency specific microcurrent.
Patients who respond positively to the non-invasive treatments via a dramatic decrease in their pain levels during their first week (‘trial week’) at the Centre are invited to complete the 10-week pain program.
Upper Cervical Procedure To Stimulate The Vagus Nerve
Dr Katinka believes that CRPS is like ‘a perfect storm’ that may arise in the presence of an underactive vagus nerve. This may occur following a neck or tailbone injury that could compromise its function. In other words, Dr Katinka believes that an injury to the CNS that could affect the vagus nerve is a major risk factor (amongst other factors) for CRPS in some patients.
Dr Katinka’s gentle hands-on upper cervical diagnostic procedure is performed on each CRPS patient during the first day of the ‘trial 1-week’. During this diagnostic test, CRPS patients are requested to lay on the treatment table. This non-invasive and painless procedure enables Dr Katinka to diagnose whether an underactive vagus nerve exists.
In Dr Katinka’s experience, most, if not all, CRPS patients present with a hypoactive vagus nerve. Furthermore, in her opinion, unless the problem in the CNS (being an underactive vagus nerve) is properly addressed, many may never get to the bottom of CRPS. In other words, if one only treats the symptoms of CRPS including pain (via pain medications, ketamine, spinal blocks, spinal cord stimulator, etc), instead of addressing the actual cause for these symptoms (such as an injury in the CNS that affects the vagus nerve), one may never be able to help CRPS patients.
Dr Katinka’s gentle manipulation of the patient’s upper cervical region often results in stimulation of the vagus nerve. In turn, this can reduce localized inflammation almost immediately that may lead to pain relief. These manipulations are repeated throughout the 10-week program, as necessary.
Thanks to Dr Katinka and her team, many CRPS patients are finally able to enjoy their lives without pain, while many more CRPS patients benefit from reduced pain and increased function and mobility.
Often dreams become reality at The Neurologic Relief Center (Spero Clinic), Arkansas, thanks to Dr Katinka and her team!
Sabina Walker
Blogger, Pain Matters (in WordPress)
REFERENCES
Other Pain Matter Blog Links and References of Dr Katinka
Frequency Specific Microcurrent And Other Non-Invasive Treatments For CRPS By Dr Katinka
Putting Out the Fire: A Brand New Approach to Treating RSD/CRPS (guest blog post, RSDSA website (12 April 2016)
http://rsds.org/new-approach-rsd-crps/
Academic References on the Efferent Vagus Nerve, Inflammation, Pain, etc
Walker, Sabina, Drummond, Peter D. Implications of a Local Overproduction of Tumor Necrosis Factor-α in Complex Regional Pain Syndrome [Review Paper]. Pain Medicine (Dec 2011); 12(12): 1784–1807 (24 pages).
http://onlinelibrary.wiley.com/doi/10.1111/j.1526-4637.2011.01273.x/abstract
Patient YouTube Links and References of CRPS Patients
- Carlos’ CRPS Story
https://www.youtube.com/watch?v=pYE0aW1cTh8 (23 January 2015)
https://youtu.be/tC_JyDfvexM (8 June 2011)
http://seeingyouwell.com/testimonials/
Putting Out the Fire: A Brand New Approach to Treating RSD/CRPS (guest blog post, RSDSA website (12 April 2016)
http://rsds.org/new-approach-rsd-crps/
- Brock’s CRPS Story
https://www.youtube.com/watch?v=MU7ggYcdJO4 (21 December 2015)
- David’s CRPS Story
Groundbreaking CRPS Treatment by Dr Katinka
https://www.youtube.com/watch?v=hWIaMBhcvA0&sns=em (30 October 2015)
- Madi’s CRPS Story
https://www.youtube.com/watch?v=IVqSGHwmf-E (7 August 2015)
- Scott’s CRPS Story
https://www.youtube.com/watch?v=3p1dOOHDuio (28 May 2016)
- Barbara Wall’s CRPS Story
My Journey Back to Health: Barbara Wall and RSD (3 May 2016)
http://rsds.org/journey-back-health-rsd/
- Brenda’s CRPS Story
http://seeingyouwell.com/testimonials/ (a 1-minute YouTube)
- Debbie’s CRPS Story
https://www.youtube.com/watch?v=yxgG6RfcrRY (27 October 2016)
- Kristin’s CRPS Story
https://www.youtube.com/watch?v=ltc8fUKhmZM (30 May 2016)
- Billi’s CRPS Story
https://www.youtube.com/watch?v=TpMSqe_aXk0 (20 March 2015)
The Wandering Nerve And CRPS
Source of Featured Image of the vagus nerve (‘the wandering nerve’).
https://en.wikipedia.org/wiki/Vagus_nerve
Dear Pain Matters blog readers,
As mentioned in earlier posts, Dr Katinka van der Merwe (aka Dr Katinka), a Doctor of Chiropractic at The Neurologic Relief Center, Arkansas, USA, specializes in chronic pain including CRPS. Dr Katinka’s unique and non-invasive approach focuses on rebalancing the autonomic nervous system, with particular emphasis on the vagus nerve (‘the wandering nerve’).

Source of photo of Dr Katinka:
https://www.facebook.com/TheNeurologicReliefCenter/?fref=mentions&pnref=stor
Dr Katinka has expertise in various non-invasive treatments including:
- Upper Cervical Procedure (to stimulate the vagus nerve); and
- Frequency Specific Microcurrent.
These (and other) treatments may be beneficial for neuropathic pain and injury to the spinal cord and other painful conditions.
This blog post discusses Jennifer, a CRPS patient who suffered pain levels up to ‘10’ on a daily basis for many years until she finally attended The Neurologic Relief Center (headed by Dr Katinka). Happily, Jennifer obtained complete pain relief following non-invasive treatments for 5 weeks at this Center.
Jennifer’s CRPS
Jennifer’s CRPS in her right foot occurred after a stress fracture to the top of her right foot in 2007/2008. Her CRPS spread to her right arm, wrist and hand. Jennifer also had spinal surgery 2 years ago that involved metal implants including a metal cage, plates and screws.
Jennifer suffered shooting and excruciating pain levels up to ‘10’, 24/7, as well as severe migraines. Her pain made it difficult to do anything including walking, working and concentrating/focusing. Her sleep was constantly interrupted by pain and she was unable to sleep with covers due to hypersensitivity. Jennifer had difficulty wearing shoes in the daytime. Needless to say, a life with severe and constant pain was very debilitating for Jennifer.
Because pain is ‘invisible’, people who had no pain could not understand her (with the exception of her supportive husband). It was hard for Jennifer to hear people tell her, ‘There’s nothing wrong with you’, when in fact she was in such agony and pain.
Jennifer tried various pain medications including Lyrica (at maximum dosages), morphine and Cymbalta. Jennifer said that while these drugs made her think that her pain was better, they did not enable her to do anything or function properly. Sadly, her pain never went away no matter how high the dosages were.
Dr Katinka’s Non-Invasive Treatment For Jennifer’s CRPS
Dr Katinka does not treat CRPS directly. In her words (quoting from both Youtubes, below):
‘The difference between how we treat RSD [CRPS], or the neurologic symptoms of RSD [CRPS], is that we do not treat pain. We do not numb the pain. We do not interrupt the pain signal. We do not attack the pain signal. We don’t try to interrupt the nerve signal … that is not what’s causing the RSD [CRPS]. The RSD [CRPS] is caused by a malfunction in the central nervous system.
We treat the central nervous system injury. And unless you treat that, you will never, ever permanently get the RSD [CRPS] under control, in my opinion.’
Dr Katinka added that many patients have injuries in their upper cervical region or tailbone area. These types of injuries may affect the vagus nerve. If left untreated, these injuries can affect the central nervous system, and in particular, the parasympathetic nervous system including the vagus nerve. Ultimately, this may trigger CRPS.
As stated above, Dr Katinka’s team offered non-invasive treatment for Jennifer’s CRPS that includes a combination of:
- An upper cervical procedure – This involves gentle hands-on treatment of the very upper cervical region to release, stimulate and activate the vagus nerve. This gentle treatment removes any pressure on the vagus nerve, hence instantly restoring vagus nerve function and reducing pro-inflammatories. When this occurs, there can be an immediate decrease in pain. This procedure is frequently repeated during the 10-week treatment period; and
- Frequency Specific Microcurrent (FSM) – This is done to treat:
- Inflammation of the spinal cord including nerves and abnormal scar tissue (from Jennifer’s spinal fusion surgery 2 years ago);
- Allergic reactions and toxicity – Jennifer’s back surgery involved metal implants in her spine including a metal cage, plates and screws. These metal implants are at risk of releasing toxins that may trigger metal allergies; and
- Stenosis (ie narrowing of the spinal canal).
Jennifer shared details of her 3rd week at the Center in the YouTube dated 26 July 2015 (see below). At this time, her CRPS-affected right foot was still swollen, compared to her unaffected foot. Furthermore, her pain levels were at ‘8’ before beginning FSM.
Jennifer confirmed that her pain vanished during FSM treatment. Instead, she had a ‘hot/warm feeling of water on the foot, with no pain’. Quoting Jennifer:
‘It feels funny … It just feels funny. I’ve been having pain for so long … You have to stop and think, ‘Look, there’s nothing [ie no pain] there.”
Pleased with Jennifer’s progress thus far, Dr Katinka stated:
‘We don’t have tissues here, do we? I must have made you cry [with happiness] … Oh, we do [have tissues].’
Jennifer added, ‘…It’s amazing … from one day to the next … how it feels…’
After FSM treatment, Jennifer practiced walking slowly down a hallway under Dr Katinka’s caring supervision. Dr Katinka stated (quoting):
‘…You’re done with your treatment … And you are walking on your foot. Can you normally walk on it?’
Jennifer answered, ‘Not very well. No. It really hurts … Yeah, this is really different…’
When Dr Katinka asked about her pain levels while walking down the hallway, Jennifer literally sang out, ‘A ‘2’!’
After 5 weeks of treatment, Jennifer’s right foot was still swollen and slightly sensitive. The good news was that Jennifer’s pain levels were now down to ZERO (ZILCH!) for the past 2 days! Wow! What fun! She was also able to sleep throughout the night now, something that she had not enjoyed for years. Woohoo!
Other CRPS Patients Successfully Treated By Dr Katinka
For dozens of other CRPS success stories, please follow the links in:
and
https://www.facebook.com/TheNeurologicReliefCenter/?fref=mentions&pnref=stor
Summary
Dr Katinka’s non-invasive combination treatment that focuses on rebalancing the autonomic nervous system including vagus nerve may offer pain relief and improved function for some chronic pain patients including CRPS patients.
For more on Dr Katinka’s unique insights into CRPS, please click her following guest blog post on the RSDSA website:
Putting Out the Fire: A Brand New Approach to Treating RSD/CRPS (12 April 2016)
http://rsds.org/new-approach-rsd-crps/
Thanks to Dr Katinka and her team, Jennifer is finally able to enjoy her life without painful CRPS!
Sabina Walker
Blogger, Pain Matters (in WordPress)
REFERENCES
Jennifer’s CRPS Story – 2 YouTubes by Dr Katinka van der Merwe
(1A) Jennifer’s CRPS Story (26 July 2015) (6-minute YouTube)
(1B) Jennifer’s CRPS Story (continued on 10 August 2015) (8-minute YouTube)
https://www.youtube.com/watch?v=PLkqMzLv9Xw
Frequency Specific Microcurrent for Pain
(2A) McMakin, Carolyn. Frequency Specific Microcurrent in Pain Management (3 December 2010); Pages 1-256.
eBook ISBN: 9780702049255
Paperback ISBN: 9780443069765
(2B) McMakin, Carolyn. Nonpharmacologic Treatment of Neuropathic Pain Using Frequency Specific Microcurrent. The Pain Practitioner (2010); 20(3); 68-73.
(2C) Thomas, Brooke. Carolyn McMakin: The Resonance of Repair (A 68 Minute-Podcast Interview with Carolyn McMakin). Liberated Body (23 December 2014); LBP 030.
(2D) Treating RSD/CRPS With Frequency Specific Microcurrent (a 75-minute YouTube done 18 September 2014 by Dr Carolyn McMakin)
(2E) Other YouTubes By Dr Carolyn McMakin
Frequency Specific Microcurrent And Other Non-Invasive Treatments For CRPS By Dr Katinka
Source of Featured Image of Dr Katinka van der Merwe:
Dear Pain Matters blog readers,
As mentioned in the previous blog post, Dr Katinka van der Merwe (aka Dr Katinka) at The Neurologic Relief Center, Arkansas, USA, has expertise in various non-invasive pain treatments including Frequency Specific Microcurrent (FSM).
For more on Dr Katinka’s unique insights into CRPS, please click her following guest blog post on the RSDSA website:
Putting Out the Fire: A Brand New Approach to Treating RSD/CRPS (12 April 2016)
http://rsds.org/new-approach-rsd-crps/
Frequency Specific Microcurrent is a very small current – so small that it can not even be detected by sensory nerves. As such, it is not painful. In fact, this current is similar to the current that is naturally produced by each cell in our body.
The FSM device (now FDA-approved) is used to treat nerve pain and injury to the spinal cord as well as many other chronic and painful conditions (see References). Its co-founder and FSM expert, Dr Carolyn McMakin, even used this system to successfully treat her own son for CRPS.
Sunday’s Treatments For CRPS Including Frequency Specific Microcurrent (FSM)
Sunday is a welder by trade who lives with her young daughter in Texas. Sunday used to enjoy an active life that included basketball and softball.
Unfortunately, Sunday had a motor vehicle accident (MVA) that involved rolling her truck 6 times. Tragically, Sunday suffered severe headaches for 3 years after this MVA. Sunday said that her intense headaches affected 7 areas in her head including the right side, adding that they felt like a knife going in and out of her head.
Shortly after her MVA, Sunday developed severe CRPS that affected her right hand to above her right elbow. Even a light touch on her right arm was excruciating. Sunday also had complete numbness in all 3 middle fingers in her right hand as well as some swelling in her right forearm and hand.
Sunday stated that her severe pain never went away after her MVA, with the exception of 3 days of relief obtained during a nerve block done to the back of her head. Her pain levels were always ‘5’ or greater, regardless of her pain treatment. Sunday also tried epidurals (where her entire right arm was numbed), Botox injections, electroshock therapy, topical pain medications, acupuncture and many more pain treatments. Sadly, nothing helped. Sunday stated that her severe and unrelenting pain was starting to affect her mental state.
In 2015, Sunday travelled interstate from Texas to Arkansas in the hope that she might find some pain relief at The Neurologic Relief Center, headed by Dr Katinka. Dr Katinka’s non-invasive treatments were different from Sunday’s other pain treatments to date. This is because Dr Katinka focused on treating the original injury caused by her car accident. In Dr Katinka’s view, Sunday likely sustained an injury to her upper cervical region during her motor vehicle accident that may also have led to CRPS in her right arm.
Following treatment of her injured upper cervical spine on her first day, Sunday’s pain levels dropped to a ‘4’. After her 2nd day of treatment, Sunday’s pain dropped further to a ‘3’. On her 3rd day of treatment, Sunday’s pain was a ‘4’ prior to undergoing FSM.
Guess what happened next??
During her 1st FSM treatment on her 3rd day, Sunday started to feel some tingling in her 3 fingers! Wow!! (Until now, Sunday had endured 3 years of numbness in these 3 middle fingers, post-MVA.) Sunday’s pain levels also dropped to a ‘3’ after FSM. Finally, there was no more pain above Sunday’s wrist and her pain was now limited to the base of her wrist following her successful FSM therapy.
In Sunday’s words,
‘It does not hurt [above the wrist] … It’s awesome … It’s awkward … It’s weird … Just my joints are sore, but everything else is not [sore] …’
Thus, Sunday felt more than 50% better within only 1 week of treatment at The Neurologic Relief Center! Sunday’s pain due to CRPS was now limited to her right wrist only and a tingling sensation had finally returned to her 3 fingers for the first time after 3 years of numbness following her MVA. The swelling in her right arm was also reduced.
Sunday’s first week at The Neurologic Relief Center offered hope that a life with less pain and greater right hand function was now possible! Sunday was excited about completing the full 10-week treatment program at this Center shortly.
Other CRPS Patients Successfully Treated By Dr Katinka
For dozens of other CRPS success stories, please follow the links in:
and
https://www.facebook.com/TheNeurologicReliefCenter/?fref=mentions&pnref=stor
Summary
Frequency Specific Microcurrent may offer pain relief and improved function for some chronic pain patients including CRPS patients. As such, FSM warrants further investigation (see References for papers by FSM expert, Dr Carolyn McMakin).
It is heart-warming to see that some CRPS patients such as Sunday are finally getting their lives back thanks to passionate and compassionate Pain Doctors including Dr Katinka!
Sabina Walker
Blogger, Pain Matters (in WordPress)
REFERENCES
Sunday’s CRPS Story – 3 YouTubes by Dr Katinka van der Merwe
(1A) Sunday’s 1st Day of Treatment for CRPS (16 March 2015)
https://m.youtube.com/watch?v=6oS-_tZRcmQ
(1B) Sunday’s 3rd Day of Treatment for CRPS (18 March 2015)
https://www.youtube.com/watch?v=nf_3GoygF4s
NB This YouTube includes a discussion of Frequency Specific Microcurrent (FSM).
(1C) Sunday’s 5th Day of Treatment for CRPS (20 March 2015)
https://m.youtube.com/watch?v=Ddl-iXxpJDU
Frequency Specific Microcurrent (FSM) for Pain
(2A) McMakin, Carolyn. Frequency Specific Microcurrent in Pain Management (3 December 2010); Pages 1-256.
eBook ISBN: 9780702049255
Paperback ISBN: 9780443069765
(2B) McMakin, Carolyn. Nonpharmacologic Treatment of Neuropathic Pain Using Frequency Specific Microcurrent. The Pain Practitioner (2010); 20(3); 68-73.
https://frequencyspecific.com/microcurrent-experimental-results-5407/about/
https://frequencyspecific.com/faq/
(2C) Thomas, Brooke. Carolyn McMakin: The Resonance of Repair (A 68 Minute-Podcast Interview with Carolyn McMakin). Liberated Body (23 December 2014); LBP 030.
https://www.liberatedbody.com/podcast/carolyn-mcmakin-lbp-030
(2D) Treating RSD / CRPS With Frequency Specific Microcurrent (a 75-minute YouTube done 18 September 2014 by Dr Carolyn McMakin)
https://www.youtube.com/watch?v=hdIGVjrZ6aQ
(2E) Other YouTubes By Dr Carolyn McMakin
“Happy Disabiliday!” A Letter To You All From Paula Orecklin, A CRPS Patient From Canada
Featured image and photo credit: Dario Schor
You may remember Paula Orecklin, the inspirational Canadian CRPS patient whom I wrote about in yesterday’s blog post:
Let’s Talk To An Inspirational Young Canadian Woman, Paula Orecklin, About CRPS, Sativex, Physiotherapy and Neuroplasticity
(There are additional References and Links at the end of this blog post.)
This week, Paula sent me a beautiful letter to share with all of you (see below). Paula’s letter contains a very important message for everyone, on behalf of all people living with disabilities including chronic pain.
I feel delighted and honoured that Paula decided to share her inspiring letter and beautiful photos with my Pain Matters Blog (as well as any other media that Paula chooses).
Upon reading Paula’s letter, I thought to myself,
“Paula’s idea to start a ‘Disabiliday‘ tradition for patients whose lives are challenged by disability and pain is fabulous! In fact, any day, whether it is April 1 or otherwise, is a great day to celebrate people who face adversities and obstacles due to disability including pain, and to also be grateful for our own blessings.”
Quoting from Paula’s her own words written to all of you from the bottom of her beautiful, caring and generous heart:
“This past Saturday, April 1, 2017, I held the world’s newest disability holiday – Disabiliday. I just entirely made up a holiday. I figure someone has to have started every other celebration, so why can’t I do the same?
Last year, I had my 15th anniversary of having Complex Regional Pain Syndrome, a severe chronic pain disease. With such a large milestone, I knew I could either get very depressed, or make something positive out of it. It wasn’t something I could just ignore. Instead, I chose to make a celebration out of it. I hadn’t just been in pain for 15 years – I was in pain for 15 years and was still going.
It became my Disabiliday.
The event turned out to be so positive and wonderful that I decided to hold a second one this year. I ended up making more progress this past year than I ever had, in terms of function and ability. I wanted to celebrate that as much as anything – that I’ve been in pain for 16 years and am now going somewhere. I don’t really know where yet, but I figure I have another year to figure that out.
I think Disabiliday could also be relevant to other people with disabilities. When you’re disabled, you can often feel isolated, or like you’re not having the same kind of lifetime milestones other people have. Maybe you can’t move out and have a housewarming, or maybe you can’t have a long term relationship with engagement and marriage and babies. Of course, plenty of people with disabilities do just those things and I’d never discount them or their lives – but I, at least where I am right now, don’t feel like I’m able or ready for them. And even birthdays can feel like you aren’t where you should be in life, especially compared to people around you.
So I wanted to do something new and different. I wanted something that fit where I am in life, where I am emotionally.
And thus, Disabiliday. A day to celebrate that despite the amount of pain I’m in, despite the limitations my disease has enforced, I still am. I still have worth. I still have a presence in people’s lives. I still am going.
Surrounding myself with the support structure I’ve been so lucky and honoured to have found in my life, I was able to sit back and take in just how many people love and care about me. Without them, I would never have gotten through so many years of pain. They’ve made the time worth it.
Disabiliday is a way of reinforcing my place in life. The place in my life, and in my family and friends’ lives. Emotionally and psychologically, all of the normally invisible ways people care were made evident. It might seem silly to just make up a holiday out of nothing but a terrible pun my friend came up with to have a Disabilitea Party that I later expanded because if I’m going to make up a celebration I might as well get a full day out of it, but the meaning really is there.
And it was a lot of fun too. I got my hair and makeup done at Sephora and Mario’s Salon (now Aura Polo Park) respectively last year and felt amazing once I was all made up. This year I got my hair highlighted, trimmed, and makeup all done at Aura Garden City. It’s superficial to some extent, but I felt so much better once finished. It’s an external thing, of course, but that doesn’t mean it doesn’t matter.
Last year we went to Sam Po Dim Sum and also introduced all of my non-Jewish Winnipegger friends to the deliciousness that is a shmoo torte from Gunn’s Bakery. It’s this layered angel food and whipped cream confirmation that’s North End of Winnipeg Jewish tradition.This year I upped my game with a wonderful dinner at Kildonan Park’s Prairie’s Edge restaurant and a cane cake from Dolce Bake Shop.
I’ve used two canes for quite a few years now (when I wasn’t in a wheelchair), and I’m finally, finally starting to walk on my own. In fact, I made a great entrance to my party by walking in. That alone made the night amazing.

Photo Credit: Dario Schor
But I wanted to step it up. I went to this awesome bakery (I recommend the chocolate cupcakes with pistachio buttercream icing) and had the pastry chef make a custom cake for me- a replica of one of my canes.
And man, did slicing that thing up feel good!

Photo Credit: Dario Schor
Other highlights of this year’s Disabiliday party included a featured guest, my physiotherapist Maria Pawlyshyn of Movement360 Inc. She is a huge part of why I’ve made so much progress this past year. Working with her, I’m doing better than I ever have since developing Complex Regional Pain Syndrome.
Other features included a dinosaur balloon- a DisabliT-rex of course (I hate myself for these puns just as much as you do) – and a truly stunning purse my mom and I designed and she made for the event (see top photo). We’ve made a lot of purses over the years, but this one has to be one of the best. Just really gorgeous. The writing on the front of it is my handwriting.

Photo Credit: Dr George Fulford
We also filmed the Disabiliday parties for a documentary Dr. George Fulford of the University of Winnipeg and I have been filming for a few years now, with the assistance of Steven Mellor for sound. Originally meant to be the first of a series of five minute videos of young adults with disabilities, this project has ended up capturing the huge amount of progress I’ve made over the past couple years. I was at my worst, nearly entirely wheelchair bound, when we started this project and I’ve made such huge gains. To actually walk on my own – I never expected ever to do that again in my life.
In other bragging about things news, my wonderful friends got me the most amazing sets of rings for a Disabiliday present. This isn’t quite as materialistic as you might think. For many years now, I’ve developed open sores and wounds all over my body. My doctors think that with the amount of pain I’m in, always, the skin has just sort of gotten very weak and opens up into wounds. I don’t do anything to create them, I’d like to explain – they just open up without any influence or action on my part. They eventually close up but leave scars. Even though the scars eventually start to fade, it doesn’t help because more new wounds have already opened up.
To detract attention from all of my wounds, I wear lots of rings (and wear makeup) to both cover up wounds on my fingers and to attract attention away from wounds on the rest of me. My friends know this, and so rings really do mean a lot to me. Plus they are adorable and I totally love them too.
So Disabiliday does really have some meaning. One one level, I realize how weird – and how self-important – it is to make up your own holiday and expect people to celebrate it. On another hand, this matters to me, and my friends honestly do support it. If it makes me feel better, if it doesn’t harm anyone else…why not? Maybe a lot of people – if they were to ever even hear about it – will think me stuck up or even that I’m celebrating being a victim of my disease, but I can’t help that. All I can do is lay out my reasoning here and hope maybe other people might understand. That’s really all anyone can ever do, really.
Finally, I want to thank Prairie’s Edge for hosting us, Dolche Bake Shop for a delicious cane, and Aura Garden City for totally making me over.
And I really want to thank my best friend, Eryn Schor, for not only organizing both of my Disabiliday events, but actually sticking around for the better part of five hours as I got all made up. Now there is a truly loyal friend! She means so much to me and has been by my side since we met in elementary school. Without her, these events would never have happened.
Thanks also go to Dr. George Fulford for filming the whole event – and for filming my life over the past few years, and to Steven Mellor on sound. Dealing with that boom mike was not easy!
And lastly, thanks to my parents. My dad was unable to be in town for the event, so we just got him on Skype on a phone to take some family photos. With my parents, all of my friends, and my health care providers, with all of their love, care, support, understanding, work, and through their thought, research, and education, I can truly say that despite the amount of pain I’m in, the past 16 years have been entirely worth it.
Happy Disabiliday!”

Photo Credit: Dario Schor
I am certain that most of you will be equally touched by Paula Orecklin’s letter just as I am!
Sabina Walker, Pain Matters Blogger
PS Are there any thoughts on Paula’s idea of a ‘Disabiliday‘ tradition from the rest of you in ‘Pain Matters Blog Reader-Land’? If yes, please feel free to comment…
FURTHER REFERENCES AND LINKS ON PAULA ORECKLIN, CRPS PATIENT:
(1) Paula Orecklin – UNE Patient Case Study – April 4, 2013
https://www.youtube.com/watch?v=_aAVOCGW5ac
(2A) CRPS Video on CRPS by PARC (a CRPS website)
https://painmatters.wordpress.com/2014/10/26/crps-video-on-crps-by-parc-a-crps-website/
(2B) This blog post also includes details and links to a video/DVD called:
Living a Life in Pain – The Story of RSD/CRPS (by Sarah Panas, film maker):
http://www.rsdcanada.org/parc/english/parc/news.htm
This video is also accompanied by a 5-minute trailer:
Living a Life in Pain: The Story of RSD/CRPS – Trailer’