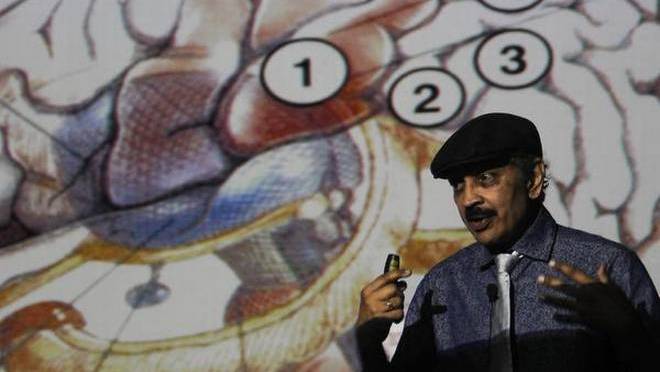
Feature Image of Professor Ramachandran sourced from:
https://www.thehindu.com/news/cities/chennai/Demystifiying-a-phantom/article17009821.ece
Thanks to Professor Ramachandran’s inspiring research into mirror therapy, the world is now a better place for many amputees with phantom limb pain and other patients!
For related blog posts, see:
https://painmatters.wordpress.com/2019/02/18/mirror-therapy-what-your-eyes-see-is-reality
Dear Pain Matters blog readers,
This blog post discusses:
- A clinical trial involving mirror therapy;
- Two (2) amputees who had successful mirror therapy for phantom limb pain; and
- Professor V.S. Ramachandran’s ground-breaking research into mirror visual feedback via mirror therapy.
Phantom pain affects at least 90% of all amputees. It includes a myriad of painful sensations including the following:
- The limb feels frozen in an awkward position;
- Burning;
- Stabbing;
- Shooting; or
- Electrical shocks.
The good news is that mirror therapy (aka mirror visual feedback) may offer a cheap and effective treatment option for some amputees with phantom limb pain and other pain sufferers.
WALLACE FANENE, THE EXPLOSION AND THE TRAUMATIC LOSS OF 2 LIMBS
Sgt. Wallace Fanene’s Story
Sgt. Wallace (‘Wally’) Fanene, a 25-year old Samoan in California, was severely injured on September 8, 2007, while serving in Iraq. He lost both his right arm and his right leg in an improvised explosive device (IED) blast. At first, Wally did not feel any pain, although he had a burning sensation in his injured legs. In his words,
‘I knelt down on a landmine; I sat on it. I knew my leg was gone right when I was hit, but I didn’t feel any pain, and I didn’t know about my arm.’
Things got even weirder at the hospital when Wally asked his wife to scratch his bandaged right hand to relieve itching. What Wally did not realise was that his lower right arm was also missing!
‘[My wife] told me my arm was gone. We argued about that for five minutes. I mean, I could feel it.’
It was at the hospital when the pain kicked in big time, even affecting his sleep. There were nails in his phantom toes as well as needles and a knife-like pain in his missing leg.
Wally added,
‘It was the most excruciating pain in my life.’
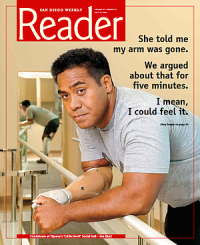
Source: https://www.sandiegoreader.com/news/2008/jul/09/cover/
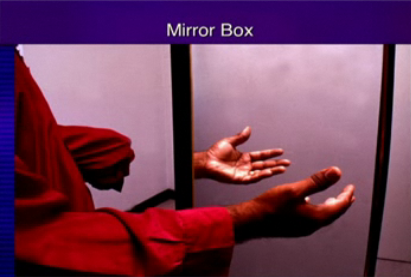
Enter Mirror Therapy
Not knowing what to expect, Wally enjoyed immediate pain relief as soon as he started mirror therapy.
In Wally’s words,
‘I was sceptical at first, but then I said, what the heck. So we tried it and [mirror therapy] worked right away. The pain just stopped. Four hours later the pain came back again, and again the mirror helped right away …
… The pain still comes back, but it’s nowhere as bad as it was. It comes back several times a day. But if [the phantom limb pain] starts to bother me, I use the mirror.’

Wallace Fanene, double amputee, and his wife
A CLINICAL TRIAL INVOLVING MIRROR THERAPY
Overview
Inspired by Professor Ramachandran’s ground-breaking research into mirror visual feedback in the mid-1990’s, Jack Tsao, Neurologist, offered mirror therapy for his patients who suffered phantom limb pain.
Soon after, Tsao set up a clinical trial involving mirror therapy for phantom pain at the Uniformed Services University in Maryland.
Specifically, 22 lower limb amputee patients with phantom pain from Walter Reed Army Medical Center (WRAMC) were randomly allocated to 1 of 3 groups. Four (4) patients were unable to complete this study.
The 1st group (N=6) received mirror therapy. The remaining 2 groups underwent covered mirror treatment (N=6) and mental visualisation (N=6).
Each group was instructed to do their assigned therapy for 15 minutes daily for 4 weeks.
This study found that ALL 6 amputees in the first group who received mirror therapy enjoyed reduced phantom limb pain after one month! Some even experienced complete relief from phantom pain after mirror therapy.
In comparison, half of the 2nd group who received covered mirror treatment and 2/3 of the 3rd group who performed mental visualization exercises had increased pain after 1 month.
Nine (9) amputees from the 2nd and 3rd groups were subsequently re-assigned to classical mirror therapy for 4 weeks. Eight (8) of these 9 amputees (89%) enjoyed less pain thereafter.
The first group performed 4 additional weeks of mirror therapy, totalling 8 weeks. This resulted in further improvements for all 6 participants.
Jack Tsao, Neurologist, said that the results ‘astounded me … I didn’t expect [the results] to be that good.’
Mirror therapy is now available at 3 US military amputee centres including WRAMC as well as other locations for amputees and patients with other painful conditions (Chan et al, 2007; Dobyns, 2008).
Nick Paupore, Amputee and Participant in Above Trial
Nick Paupore (32), a participant in the aforementioned trial, enjoyed significant relief from excruciating phantom pain following mirror therapy.
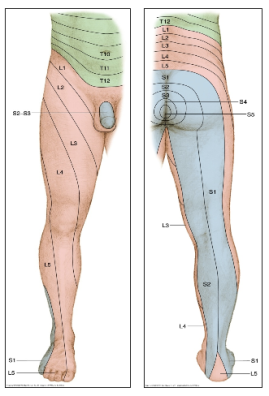
Nick lost his lower right leg in Iraq when a roadside bomb hit his vehicle. While he felt a burning sensation in the back of his legs, Nick did not feel any pain. Unfortunately, the blast tore out a chunk of his leg including 15cm to 20cm of an artery that almost caused him to bleed to death.
At the hospital, Nick suffered excruciating phantom pain in his missing leg 5 – 6 times an hour, with each bout of pain lasting up to a minute. As he screamed and dry-heaved, the searing shock raced from the missing sole in his foot up the back of his phantom calf and into his thigh.
Quoting Nick,
‘I was laying in bed and it just, all of a sudden, it felt like I was getting shocked. I called the nurse, ’cause I was like, ‘What’s going on?’
The nurse told Nick that it was likely his phantom pain.
Nick continued,
‘All of a sudden, it was like someone kept turning on and off the Taser, and my whole leg started twitching. … I sat up, and I was holding on to my stump, and it just wouldn’t stop.’
‘It was like sticking my finger in a light socket. … getting electrocuted.’
‘… the [phantom] pain was driving me insane.’
And now for the good news:
Nick was almost pain-free after mirror therapy for a month. Furthermore, he no longer needed pain medication 5 months later.

Jack Tsao, Neurologist, with Nick Paupore during mirror therapy
http://www.dana.org/QA/Mirror_Therapy_for_Phantom_Limb_Pain/#_ftn2
Quoting Tsao, Neurologist,
‘The difference is like night and day … To see him walking, he’s able to drive his car; he works downtown; I mean, that is incredibly gratifying!’ (Burgess, 2008; Young, 2008).
SEMINAL RESEARCH BY PROFESSOR RAMACHANDRAN
Overview
Professor Ramachandran did research in the mid-1990’s based on amputees who had lost their limbs many years earlier. His studies led to mirror therapy as a pain treatment option for phantom limb pain and other painful conditions.

Neuroscientist V.S. Ramachandran
Source: https://greatergood.berkeley.edu/article/item/do_mirror_neurons_give_empathy
Many ground-breaking research findings were reported by Ramachandran including:
(1) An amputee named ‘D.S.’ lost his left arm 9 years ago. His phantom arm felt as if it was ‘frozen … in a cement block’. Ramachandran offered mirror therapy involving bilateral mirror-symmetric movements. During this therapy, D.S. felt movement in the muscles and joints of his phantom arm while looking at his intact arm in the mirror.
When Ramachandran removed the mirror, D.S. was no longer able to feel his phantom arm move. In his words, ‘It feels frozen again.’
This experiment demonstrates the importance of visual feedback via mirror therapy in restoring movement in ‘frozen’ phantom limbs. This movement may even be a prerequisite before phantom limb pain can be reduced or eliminated altogether.
(2) A left arm amputee known as ‘R.T.’ (55) suffered a paralysed phantom arm. His left hand often had clenching spasms with ‘fingernails digging into the palm’.
Mirror visual feedback was done to provide an illusion of a restored left arm. The reflection of his intact right arm in the mirror provided the visual feedback that R.T. desperately needed before he could finally ‘unclench’ and ‘move’ his paralysed phantom arm in a mirror-symmetric manner.
(3) Five patients suffered painful ‘clenching spasms’ in their phantom hand. Following mirror therapy, 4 of 5 patients were finally able to ‘open’ their phantom hand leading to relief from painful spasms.
Mirror therapy may lead to new connections in the brain. This may include novel and/or reactivation of pre-existing neural pathways between both cerebral hemispheres (Ramachandran & Hirstein, 1998).
Graded Mirror Therapy vs Traditional Mirror Therapy
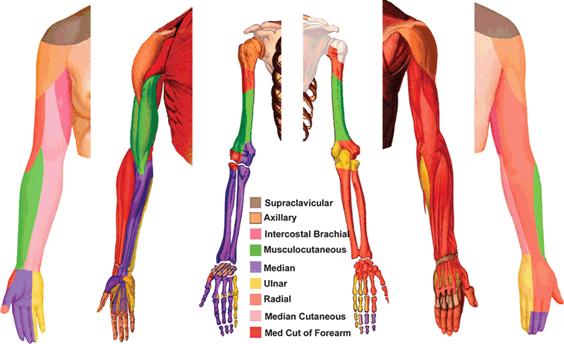
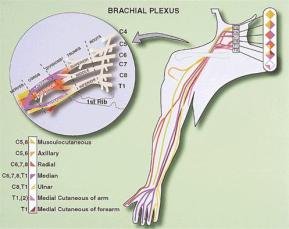
A male patient (43) suffered deafferentation pain in his right arm following brachial plexus avulsion due to a traffic accident 23 years ago. Specifically, he endured severe tingling pain including numbness in his right fingers (pain rating of 10/10).
Traditional mirror therapy for 4 weeks failed to offer pain relief.
Graded mirror therapy, on the other hand, ultimately led to complete relief from pain.
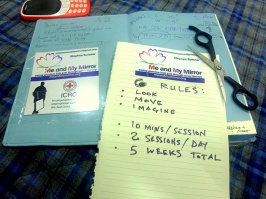
Graded mirror therapy comprises 5 steps, being:
- Observing the mirrored reflection of the unaffected side without imagining any movements in the amputated limb;
- Observing the mirrored reflection of the 3rd and 4th fingers while slowly moving them from a flexed position to an extended position;
- Observing the mirrored reflection of the unaffected side during passive movements;
- Motor imagery of the affected fingers while observing the mirrored reflection of the unaffected side; and
- Motor imagery of the affected fingers without a mirror.
Graded mirror therapy involving the aforementioned 5 steps was done for 3 – 4 weeks.
The good news is that during graded mirror therapy, pain levels decreased and finally disappeared altogether. The patient was also able to imagine finger movement both with and without a mirror (Mibu et al, 2016).
Possible Mechanisms
Although there is no shortage of possible explanations, no one really knows why mirror therapy may work better in some patients than in others.
Professor Herta Flor, Neuroscientist, believes that both peripheral input and central changes may be involved in phantom limb pain (Perur, 2014).
Competitive interaction may arise between the two brain hemispheres in stroke patients (and presumably also in amputees). This can lead to abnormal interhemispheric inhibition (IHI) and weakened motor function.
In stroke patients, mirror therapy and motor training could increase the excitability of the stroke-affected primary motor cortex (M1). Specifically, mirror visual feedback training could alter the excitability of the transcallosal pathway and restore IHI back to normal. This could in turn strengthen motor function in the stroke-affected side.
Thus, mirror visual feedback training may help normalise IHI and restore the hemispheric balance between the stroke-affected (or amputation-affected) M1 and the healthy M1 (Avanzino et al, 2014).
Another study reported that mirror visual feedback via a mirror led to improved motor function in 2 patients who had callosal disconnection. Based on this, they concluded that mirror therapy that leads to improved motor performance does not affect interhemispheric interaction via corpus callosum (Nojima et al, 2013). Whether this also occurs in amputees is unknown.
See 5-minute TED-Ed Animations video called ‘The fascinating science of phantom limbs’ by Joshua Pate.
Some Questions to Ponder
Could an amputation lead to abnormal IHI and a hemispheric imbalance between the amputation-affected M1 and the healthy M1?
If yes, could this contribute (in part or in full) to ‘painfully frozen limbs’, ‘paralysed phantom limbs’ and phantom limb pain in amputees?
If so, could mirror visual feedback training using mirrors reduce phantom limb pain and other symptoms in some amputees?
Another Question
In my blog post called:
A Doctor and a Nurse who can Literally Feel Pain in Other People,
we learn that Dr Joel Salinas, a neurologist, has mirror touch synesthesia. This means that he can literally feel his patients’ pain and tactile sensations. Automatically triggered by sight, he said that, for example, when he sees someone’s right arm being touched, he also feels a touch on his own left hand – just like in a mirror.
Could Dr Salina’s experience with mirror touch synesthesia offer certain insight into why mirror therapy may offer relief from phantom limb pain in many amputees?
SUMMARY
Mirror therapy including graded mirror therapy may be a very effective treatment option for amputees with phantom limb pain and other chronic pain sufferers.
Benefits derived from mirror therapy vary from one patient to the next. According to Professor Christoph Maier, while some amputees are pain-free after only 1 mirror therapy session, others may need to do mirror therapy for the rest of their lives to reduce phantom pain (Liebling, 2010; translated from German).
Who would have thought that a humble mirror could offer relief from excruciating phantom limb pain for some amputees??
Sabina Walker
Blogger, Pain Matters (in WordPress)
REFERENCES
Patient Stories
(1) Dobyns, Stephen. Certain San Diegans feel their missing limbs. San Diego Reader (9 July 2008).
(2) Saundra Young. For amputees, an unlikely painkiller: Mirrors. CNN (19 March 2008).
http://www.cnn.com/2008/HEALTH/03/19/mirror.therapy/index.html
(3) Burgess, Lisa. Mirrors helping amputees fight phantom pain. Stars and Stripes (2/2/2008).
https://www.stripes.com/news/mirrors-helping-amputees-fight-phantom-pain-1.74351
(4) Colapinto, John. Brain Games – The Marco Polo of Neuroscience. The New Yorker (11 May 2009).
https://www.newyorker.com/magazine/2009/05/11/brain-games
Peer-Reviewed Science Papers
(5) Chan BL et al. Mirror therapy for phantom limb pain. N Engl J Med (22 Nov 2007); 357: 2206-2207.
doi: 10.1056/NEJMc071927
https://www.physio-pedia.com/images/1/11/Mirror.NEJM.pdf
(6) Uniformed Services University of the Health Sciences. Phantom Limb Pain May Be Reduced By Simple Mirror Treatment. Science Daily (24 November 2007).
http://www.sciencedaily.com/releases/2007/11/071123195218.htm
(7) Ramachandran VS & Hirstein W. The perception of phantom limbs. Brain (1998); 121: 1603-30.
http://www.rctn.org/bruno/psc129/handouts/rama2.pdf
(8) Avanzino et al. Training based on mirror visual feedback influences transcallosal communication. Eur J Neurosci (Aug 2014); 40(3): 2581-8.
doi: 10.1111/ejn.12615.
(9) Nojima et al. Mirror visual feedback can induce motor learning in patients with callosal disconnection. Exp Brain Res (May 2013); 227(1): 79-83.
(10) Perur, Srinath. The mirror man. mosaic (7 July 2014).
https://mosaicscience.com/story/mirror-man/
(11) Mibu et al. Successful Graded Mirror Therapy in a Patient with Chronic Deafferentation Pain in Whom Traditional Mirror Therapy was Ineffective: A Case Report. Pain Practice (April 2016); 16(4): E62-E69.
https://doi.org/10.1111/papr.12431
https://onlinelibrary.wiley.com/doi/full/10.1111/papr.12431
Non-Fiction Book
(12) Ramachandran VS & S Blakeslee. Phantoms in the Brain – Human Nature and the Architecture of the Mind. HarperCollins Publishers (20 May 1999); pages 1 to 352.
ISBN 9781857028959
(13A) Ramachandran VS. The Tell-Tale Brain – A Neuroscientist’s Quest for What Makes Us Human. W.W. Norton & Co (5 April 2012); pages 1 to 357.
ISBN: 9780099537595
(13B) V.S. Ramachandran’s Tales Of The ‘Tell-Tale Brain’. NPR (14/2/2011).
https://www.npr.org/2011/02/14/133026897/v-s-ramachandrans-tales-of-the-tell-tale-brain
Medical Articles (in German)
(14) Mit der Spiegeltherapie sind Schmerzen “verlernbar”. Ärzte Zeitung online (22.02.2010).
(15) Liebling, Patricia. Spiegeltherapie hilft gegen Phantomschmerzen. Aachener Zeitung (27 Feb 2010).
(16) Hawlik, Michaela. Leben mit Phantomschmerz. My Handicap (1/2011).
Other Medical Articles (not discussed in this blog post)
(17) Peterzell, David H. Psychophysical investigations into Ramachandran’s mirror visual feedback for phantom limb pain: video-based variants for unilateral and bilateral amputees, and temporal dynamics of paresthesias. 2016 Society for Imaging Science and Technology (Feb 2016).
doi: 10.2352/ISSN.2470-1173.2016.16HVEI-093
https://www.ingentaconnect.com/contentone/ist/ei/2016/00002016/00000016/art00045?crawler=true
(18) Timms, Jason & Carus, Catherine. Mirror therapy for the alleviation of phantom limb pain following amputation: A literature review. International Journal of Therapy and Rehabilitation (March 2015); 22(3): 135-145.
https://www.magonlinelibrary.com/doi/pdf/10.12968/ijtr.2015.22.3.135
(19) Datta & Dhar. Mirror therapy: An adjunct to conventional pharmacotherapy in phantom limb pain. J Anaesthesia Clin Pharmacol (Oct-Dec 2015); 31(4): 575–578.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4676260/
(20A) Ol, Ha Sam et al. Mirror therapy for phantom limb and stump pain: a randomized controlled clinical trial in landmine amputees in Cambodia. Scandinavian Journal of Pain (3 July 2018); 18(4): 603-610.
https://www.ncbi.nlm.nih.gov/pubmed/30207289
(20B) Ol, Ha Sam et al. Mirror therapy: Curing phantom pain in landmine victims. Science Discoveries (26.10.2018).
https://sciencediscoveries.degruyter.com/mirror-therapy-curing-phantom-pain-landmine-victims/