Feature Image sourced from:
https://pixabay.com/en/diving-air-oxygen-kringel-air-ring-378214/
Dear Pain Matters blog readers,
INTRODUCTION
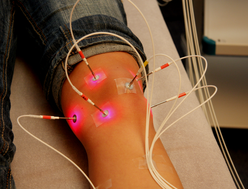
Hyperbaric oxygen therapy (HBOT) involves the delivery of 100% oxygen at increased atmospheric pressures inside a pressure chamber.
Pressures greater than normal air pressure (i.e. 1 Atmosphere Absolute, or 1 ATA) may be offered by trained personnel. Many patients are exposed to 2 to 2.4 ATA per session. Each session may last 1.5 to 2 hours and patients may complete a total of 20 to 30 HBOT sessions.
For those of you who have scuba dived, free dived or snorkelled, 2 ATA is the pressure that one would feel 10 meters (33 feet) under the ocean. Thus, every 10 meters (33 feet) of sea water is equivalent to an increase of 1 ATA of pressure.
http://www.vhbo2.com/companion/hyperbaric-oxygen-therapy/understanding-hbot/

Source:
Also called hyperbaric medicine or hyperbaric treatment, HBOT can increase oxygen concentration, reduce inflammation and decrease the number and sensitivity of tender and painful points.
This is a cute 2-minute video of a dog inside a pressure chamber (with great background music):
Hyperbaric oxygen therapy can alleviate chronic pain in:
- Complex regional pain syndrome;
- Fibromyalgia;
- Myofascial pain syndrome;
- Idiopathic trigeminal neuralgia;
- Migraines and cluster headaches; and
- Other pain conditions (Yildiz et al, 2006; Yildiz et al, 2006; Efrati et al, 2015)
as well as reduce pain following crush injuries.
PAINFUL CONDITIONS TREATED BY HYPERBARIC OXYGEN THERAPY
LOWER LIMB COMPLEX REGIONAL PAIN SYNDROME (CASE 1)
A 41-year old man, ‘G.G.’, suffered from Complex Regional Pain Syndrome Type 2 (CRPS Type 2), left foot, caused by a traumatic ‘Weber B’ left ankle fracture that occurred more than a year ago on 21 February 2014. Specifically, G.G. slipped and fell on ice in a parking lot at the end of a working day. He immediately suffered severe pain in his left ankle and foot.
Two days later, on 23 February 2014, G.G. had surgery involving open reduction internal fixation of his ankle. Complications set in including a cellulitis infection that was treated with antibiotics.
Post-surgery, G.G. endured ongoing and severe pain including intermittent shooting pains and severe electric shocks in his left ankle and foot. Other symptoms included allodynia, swelling, temperature changes and discoloured skin in the left lower limb.
Despite undergoing a rehabilitation program and taking pain medication including pregabalin (75 mg twice daily), acetaminophen and NSAIDs (as needed), multivitamins, calcium, magnesium and glucosamine, G.G.’s severe pain persisted.
A diagnosis of CRPS, left foot, was made in April 2014.
On 5 February 2015, almost one year after his injury, G.G. had surgery to remove the plateau in his left lower limb in an effort to relieve his pain. Sadly, G.G.’s symptoms including pain and allodynia, swelling, purple discolouration, lower skin temperature as well as muscle weakness in his left lower leg and ankle continued. With average pain levels at 6 that often rose to 8, G.G. described his pain as (quoting) ‘constant, dull, aching pain with intermittent shooting sensations’.
Desperate for some pain relief, G.G. decided to try HBOT for his CRPS in his left foot.
After 15 HBOT sessions over 3 weeks, G.G. had significantly less pain and allodynia, reduced swelling, enhanced skin colour and improved range of motion in his left foot. Following 3 weeks of HBOT, G.G. was able to return to work after more than a year off due to severe left foot pain.
Hyperbaric oxygen therapy may be a valuable therapeutic option for treating chronic CRPS (Katznelson, 2016).
LOWER LIMB COMPLEX REGIONAL PAIN SYNDROME (CASE 2)
A 44-year old woman had CRPS, left foot and ankle. Her foot and ankle had restricted range of motion, appeared cyanotic and was tender and cool upon touch.
Within only 15 minutes of her first HBOT treatment, she enjoyed complete pain relief in her foot! Furthermore, her foot felt warm on palpation and (quoting her) ‘pinker than it’s been in years’. The foot remained pink and warm for 8 hours. Best of all, she enjoyed nil pain for 18 hours after her first HBOT treatment!
Following amendments to her second HBOT session on the following day, her foot became pink and warm for 1 hour as well as painless for 2 hours.
Further adjustments made to her third HBOT protocol in the following week resulted in her foot remaining painless, warm and pink for 30 hours (!) (Peach, 1995).
COMPLEX REGIONAL PAIN SYNDROME
A double-blind, randomized, placebo-controlled study compared 37 CRPS patients who had HBOT treatment against 34 CRPS patients who received normal air (Control Group). All 71 CRPS patients underwent 15 sessions inside a hyperbaric chamber.
The HBOT-treated patients enjoyed significantly less pain and edema as well as enhanced range of motion of the wrist.
Hyperbaric oxygen therapy may offer pain relief, decreased swelling and improved range of motion in CRPS patients (Kiralp et al, 2004).
FIBROMYALGIA
A study involving 60 women aged 21 to 67 who suffered fibromyalgia for more than 2 years underwent 40 HBOT sessions. These 90-minute sessions were offered 5 days a week and each session involved 100% oxygen at 2 ATA. Hyperbaric oxygen therapy led to significant improvement in all fibromyalgia symptoms including improved quality of life (Efrati et al, 2015).
MYOFASCIAL PAIN SYNDROME
A study evaluated the effects of HBOT on 20 patients with myofascial pain syndrome (MPS) compared to 10 patients in the control group. The patients in the HBOT group were offered 10 HBOT sessions over 2 weeks.
There were no complications following hyperbaric oxygen therapy. The pain threshold was significantly improved as were visual analogue scale (VAS) scores in patients in the HBOT group.
The researchers concluded that HBOT may offer benefits for patients with MPS (Kiralp et al, 2009).
IDIOPATHIC TRIGEMINAL NEURALGIA
Patients with severe nerve facial pain (i.e. idiopathic trigeminal neuralgia) were offered HBOT sessions for 10 consecutive days. Specifically, 42 patients aged 40 to 70 (8 men, 34 women) who suffered trigeminal neuralgia for 2 to 20 years were selected for this study.
The researchers concluded that HBOT treatment offered quick, dose-dependent and lasting pain relief. Thus, HBOT may be an effective treatment for some nerve pain conditions including trigeminal neuralgia (Gu et al, 2012).
MIGRAINES
Female migraine sufferers were offered either:
- 100% oxygen and nil pressure (control group); or
- Hyperbaric oxygen therapy comprising 100% oxygen and pressure.
The HBOT-treated migraineurs enjoyed some pain relief. Pain levels remained unchanged in the control group.
Hyperbaric oxygen therapy may reduce the intensity of migraines and headaches (Wilson et al, 1998).
CRUSH INJURY
Due to their traumatic nature, crush injuries can result in severe injury and pain to various body regions. Crush injuries can range from minor contusions to limbs facing amputation due to tissue necrosis.
Crush injuries may affect different tissue regions including skin, subcutaneous layers, muscle, tendons, ligaments, cartilage, vasculature including capilliaries, nerves, bones and joints. Physical trauma can lead to prolonged swelling and edema, stasis and/or internal bleeding including bleeding within myofascial envelopes. The latter may lead to increased tissue fluid pressure in the skeletal muscle compartment.
Affected tissues may become ischemic due to hypoxia if the tissue fluid pressure (edema) exceeds the capillary perfusion pressure to the muscles and nerves inside the skeletal muscle compartment.
Ongoing edema may result in increased pressure as well as severely compromised microcirculation and limited or nil oxygen transfer across the capillary endothelium. This may ultimately lead to ischemia and hypoxia.
Complex regional pain syndrome, skeletal muscle compartment syndrome and other painful conditions may develop and/or limb amputation may occur if urgent and effective treatment to prevent hypoxia and ischemia following crush injury is not provided.
Thus, time is of the essence that appropriate treatments are undertaken to reduce localised inflammation and swelling.
Importantly, hyperbaric oxygen may be used as an adjunct treatment to reverse ischemic and hypoxic conditions in crush injuries.
https://www.uhms.org/4-crush-injury-compartment-syndrome-and-other-acute-traumatic-ischemias.html
WHY MIGHT HYPERBARIC OXYGEN THERAPY WORK?
Note: This section is written for scientifically-minded readers, and may be skipped altogether by others who may not be so inclined.
Animal research shows that HBOT blocks the production of tumor necrosis factor (TNF)-α in rats with chronic constriction injury. Reduced TNF-α levels may lead to decreased nerve pain (Li et al, 2011). Local overproduction of TNF-α, on the other hand, may play a role in promoting CRPS (Walker and Drummond, 2011).
Many chronic pain conditions include an inflammatory component that may lead to tissue hypoxia, ischemia and microvascular deficits (i.e. inflammatory hypoxia). Re-oxygenation of injured or diseased tissues is a prerequisite before regeneration can occur. Therapies such as HBOT may promote tissue re-oxygenation, reversal of inflammatory hypoxia and regeneration (Perdrizet, 2017) that may lead to pain relief.
Ten divers (9 males, 1 female) underwent pressures of 1, 2, 3 and 4 ATA in a supine position for 10 minutes per pressure in a hyperbaric chamber. The Spanish study found that as the pressure increased, heart rate (HR) decreased and heart rate variability (HRV) moved into the high frequency range, especially after 2, 3 and 4 ATA. Pressure-evoked increased HRV is indicative of enhanced parasympathetic (vagal) activity (Barbosa et al, 2010). Increased parasympathetic activity including enhanced vagal tone may lead to reduced pain, decreased inflammation and other medical benefits (Walker and Drummond, 2011).
Researchers recently suggested that nerve cells may actually communicate via mechanical pulses instead of electric pulses (Fox, 2018). If true, is it possible that increased atmospheric pressures via HBOT inside a pressure chamber may lead to increased mechanical pulses? If so, could this result in increased cutaneous sympathetic vasoconstrictor activity? If yes, could this induce tissue re-oxygenation and reversal of inflammatory hypoxia in some pain patients including CRPS patients? Research is warranted.
SUMMARY
Hyperbaric oxygen therapy may offer pain relief for some pain patients.
Please ensure that HBOT is done under medical supervision only and by trained personnel. Refer to References for complications that may arise from HBOT.
Sabina Walker
Blogger, Pain Matters (in WordPress)
PS Please feel free to share your personal experience with HBOT via this blog.
REFERENCES
TEXTBOOK
(1) Undersea and Hyperbaric Medical Society (UHMS). Hyperbaric Oxygen Therapy Indications, Thirteenth Edition (April 2014).
ISBN 978-1930536-73-9
PAIN CONDITIONS TREATED BY HBOT
Complex Regional Pain Syndrome
(2A) Katznelson. Successful Treatment of Lower Limb Complex Regional Pain Syndrome following Three Weeks of Hyperbaric Oxygen Therapy. Pain Research and Management (2016); Volume 2016, Article ID 3458371, 4 pages.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4904619/
https://www.hindawi.com/journals/prm/2016/3458371/
(2B) Peach G. Hyperbaric oxygen and the reflex sympathetic dystrophy syndrome: a case report. Undersea Hyperb Med. 1995; 22(4): 407–8.
Click to access RSD-Case-Report.pdf
(2C) Kiralp et al. Effectiveness of hyperbaric oxygen therapy in the treatment of complex regional pain syndrome. J Int Med Res. (May-June 2004); 32(3): 258-62.
https://www.ncbi.nlm.nih.gov/pubmed/15174218
Fibromyalgia
(3) Efrati et al. Hyperbaric Oxygen Therapy Can Diminish Fibromyalgia Syndrome – Prospective Clinical Trial. PLoS ONE (26 May 2015); 10(5): e0127012.
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0127012
Myofascial Pain Syndrome
(4) Kiralp et al. A novel treatment modality for myofascial pain syndrome: hyperbaric oxygen therapy. J Natl Med Assoc. (Jan 2009); 101(1): 77-80.
https://www.ncbi.nlm.nih.gov/pubmed/19245076
Idiopathic Trigeminal Neuralgia
(5) Gu et al. Hyperbaric oxygen therapy attenuates neuropathic hyperalgesia in rats and idiopathic trigeminal neuralgia in patients. Eur J Pain. (2012); 16(8): 1094–105.
https://onlinelibrary.wiley.com/doi/epdf/10.1002/j.1532-2149.2012.00113.x
Migraines
(6) Wilson JR, Foresman BH, Gamber RG, Wright T. Hyperbaric oxygen in the treatment of migraine with aura. Headache. 1998; 38(2): 112–5.
https://www.ncbi.nlm.nih.gov/pubmed/9529766
Crush Injury
(1) Crush Injury, Compartment Syndrome and Other Acute Traumatic Ischemias. Undersea and Hyperbaric Medical Society (UHMS).
https://www.uhms.org/4-crush-injury-compartment-syndrome-and-other-acute-traumatic-ischemias.html
Other Pain Conditions
NB The following 2 papers are not discussed in this blog post:
(7A) Yildiz et al. Hyperbaric oxygen therapy in chronic pain management. Curr Pain Headache Rep. (May 2006); 10(2): 95-100.
(7B) Yildiz et al. Pain management and hyperbaric oxygen therapy. Therapy (2006); 3(5): 597–603.
Click to access ae1e93f42de7371a28774221967dcf67fa0e.pdf
Possible Complications
(1) Complications of Hyperbaric Oxygen Treatment. Johns Hopkins Medicine
Why Might Hyperbaric Oxygen Therapy Offer Pain Relief?
(1) Li et al. Hyperbaric oxygenation therapy alleviates chronic constrictive injury-induced neuropathic pain and reduces tumor necrosis factor-alpha production. Anesth Analg. (Sept 2011); 113(3): 626-33.
https://www.ncbi.nlm.nih.gov/pubmed/21596875
(2) Perdrizet. Chronic Diseases as Barriers to Oxygen Delivery: A Unifying Hypothesis of Tissue Reoxygenation Therapy. Adv Exp Med Biol. (2017); 977: 15-20.
https://www.ncbi.nlm.nih.gov/pubmed/28685422
(3) Barbosa et al. Effect of hyperbaric pressure during scuba diving on autonomic modulation of the cardiac response: application of the continuous wavelet transform to the analysis of heart rate variability. Mil Med. (Jan 2010); 175(1): 61-4.
https://www.ncbi.nlm.nih.gov/pubmed/20108844
(4) Sabina Walker, Peter D. Drummond; Implications of a Local Overproduction of Tumor Necrosis Factor-α in Complex Regional Pain Syndrome [Review Paper, 24 pages]; Pain Medicine (Dec 2011), 12 (12), 1784–1807.
http://onlinelibrary.wiley.com/doi/10.1111/j.1526-4637.2011.01273.x/abstract
(5) Fox, Douglas. The Brain, Reimagined. Scientific American (April 2018); 318(4): 60-67.
http://www.nature.com/scientificamerican/journal/v318/n4/full/scientificamerican0418-60.html